Kasey Gambeta, RN, MN and Andrea Chambers, PhD
Affiliations: Both Kasey and Andrea work at Public Health Ontario, Canada
Corresponding author:
Kasey Gambeta
Public Health Ontario
350 Conestoga Blvd, Cambridge, ON, N1R 7L7 Canada
kasey.gambeta@oahpp.ca
ABSTRACT
Background: The purpose of this study was to describe needs of infection prevention and control (IPAC) professionals across healthcare settings in one region of Ontario, Canada to inform priorities for the development of resources and capacity-building activities.
Methods: An open survey targeting IPAC stakeholders working in diverse healthcare settings was disseminated through multiple methods, including Public Health Ontario’s stakeholder management database. The survey was open from April 1 to June 30, 2019. IPAC inquiries documented by Public Health Ontario (PHO) staff between
April 1, 2017 and March 31, 2019 were analyzed. The data collection tools and descriptive analysis were guided by the Knowledge to Action Cycle to identify gaps, understand barriers and opportunities, and preferred strategies for learning.
Results: The survey was completed by 135 IPAC stakeholders with 56% of respondents working in long-term care and retirement homes, 13% in hospitals, 11% in primary care, 10% in home care and 10% in other settings. Respondents reported that there is a need for more support to improve practices around environmental cleaning, surveillance and routine practices; however, findings varied by setting. An important theme focused on the need for strategies to inspire and motivate stakeholders to invest in infection prevention and control. A lack of support in this area was a top barrier selected by 40% of survey respondents, and 67% expressed interest in skill development in this area. While communities of practice, common-interest networking groups, are frequently facilitated by PHO to support stakeholders, this strategy was not preferred by respondents.
Conclusions: Future efforts to enhance support for IPAC can draw on these findings to help prioritize topics, understand barriers, and align with preferred methods for capacity building.
KeyWords: Needs assessment, knowledge-to-action, infection prevention and control, gap analysis, barriers to change, knowledge translation
INTRODUCTION
As the healthcare sector addresses the challenges of responding to the Severe Acute Respiratory Syndrome Coronavirus 2
(SARS-CoV-2), the causative agent of the Coronavirus disease of 2019 (COVID-19), it has been demonstrated that the importance of standardizing and improving infection prevention and control (IPAC) is more important than ever. Although efforts are currently focused on COVID-19 control, healthcare-associated infections (HAIs) of concern continue to persist and place a burden on the healthcare system.
While there have been a number of improvements to the adoption of evidence-informed IPAC practices across healthcare settings, gaps persist. There are a number of organizations working together to reduce HAIs through the adoption of best practices in IPAC. In Ontario, the Ministry of Health (MOH) develops legislation, regulations, standards, policies and directives to support strategic directions for the Ontario healthcare system. For example, they have defined standards for organizations to have IPAC programs that include specific requirements. Local public health units provide a range of supports to healthcare organizations including a focus on outbreak management and consultation on IPAC matters as outlined in the Ontario Public Health Standards. Public Health Ontario’s Regional Infection Control Teams have specialized expertise in IPAC. This team provides scientific and technical advice on healthcare associated infections and emerging IPAC issues to the MOH, Public Health Units and directly to infection control practitioners. Within PHO, the IPAC Regional Support team model ensures IPAC coverage across the province through the placement of IPAC teams in five different regions. IPAC Regional Support teams provide support and consultation to respond to client requests and inquiries; introduce and disseminate PHO guidance resources and tools; support the implementation of IPAC initiatives to achieve best practice; facilitate networks and collaboration; and inform IPAC-related research. The work of the IPAC Regional Support Teams are guided by a number of factors including trends in IPAC inquiries; emerging issues; specific requests for support; and new best practice documents developed by the Provincial Infectious Disease Advisory Committee.
PHO’s IPAC work is influenced by the Knowledge to Action Cycle which was developed in Canada based on a review of 31 planned action theories to guide knowledge translation efforts [1]. It has been used extensively to guide needs assessments in the healthcare settings [2]. Early stages of the Action Cycle in this model emphasize the importance of focusing on gaps between current practice and recommended practice and taking the time to understand the nature of barriers and facilitators to practice change before selecting implementation strategies. The model also emphasizes the importance of involving stakeholders at all phases in the process. Therefore, to improve IPAC practices, it is necessary to have information on specific IPAC practices which stakeholders find challenging, and the barriers that are contributing to variations in practice. There has been a recognition that supporting healthcare professionals with IPAC best practices may require a behavioural science approach, acknowledging that practice change or improvement is influenced by a number of different determinants beyond knowledge and skill gaps [3,4,5]. Those who support IPAC programs have diverse educational backgrounds and responsibilities. This diversity further emphasizes the importance of understanding gaps in knowledge, skills and learning preferences that are needed to effectively build the capability and motivation of others to adopt IPAC best practices.
Relatively few studies have focused on describing the needs of IPAC stakeholders within Canada and most studies tend to focus on specific settings or practice areas, which present limitations for informing a comprehensive plan to support IPAC professionals across healthcare settings [6,7,8]. Prior to the COVID-19 pandemic, a study was conducted to describe needs of IPAC professionals across healthcare settings in one region of Ontario to inform IPAC Regional Support Team priorities for the development of further resources and capacity building. This region has 133 long-term care homes, 34 hospitals, and is a mix of rural and urban settings.
A secondary purpose was to assess participants’ perceptions of the feasibility and utility of approaches informed by the Knowledge to Action cycle to better align the development of new resources and capacity building efforts with the diverse preferences and needs of stakeholders in one region of Ontario. This needs assessment was initiated and carried out prior to COVID-19 pandemic. The results will be discussed in the context of emerging IPAC issues.
OBJECTIVES
The objectives of this needs assessment were to: identify priority IPAC practices that are most in need of improvement; describe the types of barriers influencing practice change; gather information on gaps in IPAC knowledge and skills; and describe how stakeholders currently receive information, training and advice on IPAC practices and their preferences for receiving support.
METHODS
An online survey targeting IPAC professionals in this region was disseminated through multiple methods. The goal was to reach IPAC professionals working across all healthcare sectors, including: primary care (primary care medical clinics, community clinics and support services, community health centres, First Nations and Inuit Health Branch with Indigenous Services Canada), hospitals, long-term care homes, retirement homes, dental clinics, first responders, and home care (including home and community care). The survey was distributed by email to IPAC stakeholders in PHO’s stakeholder relations management database (n = 1067). The online survey was also promoted by PHUs in the region, and the local IPAC-Canada chapter, a professional association that promotes best practices in IPAC through networking, education, and advocacy [9]. The survey was also disseminated by PHO staff at stakeholder meetings and education events. The survey was open between April 1, 2019 and June 30, 2019.
The survey collected information identifying the respondent’s sector, job title, allocation of time spent on IPAC, IPAC training received, IPAC training desired, top three practice areas most in need of improvement, types of barriers to practice change, screening and surveillance practices, reprocessing practices and training, preference for receiving information and training, current use of IPAC resources, desired IPAC resources, and interest in skill development.
Development of the survey questions was informed by best practice recommendations for IPAC and existing IPAC training and resources available. The COM-B system, a framework for understanding behaviour change [10] was used to frame questions for stakeholders about the types of barriers that affect practice change in their organization. This model includes capability (knowledge, skills), motivation (beliefs, attitudes, role clarity, intentions, buy-in, risk perception, understanding consequences), and opportunity factors (physical environment and resources, social support and leadership) [10]. The survey included mostly multiple-choice questions incorporating some minor variations to tailor the response options by sector. An open-ended question was used to collect information on barriers to practice change. An additional open-ended question was used to identify other resources PHO could offer to better support IPAC practices at the respondents’ facility.
Comments from the open-ended question about barriers were coded using predefined descriptive themes including: knowledge and skill, physical environment and resources, leadership support and culture, and motivation. Subthemes within each of these areas were then identified. Comments about resources PHO could offer in the future were grouped by setting and by common descriptive themes.
Stakeholder inquiries received by PHO from all sectors between April 1, 2017 and March 31, 2019, were reviewed. Inquiry analysis involved the identification of the most common topics within each stakeholder sector, followed by a classification of themes within those topics. Themes were compared to information collected in the survey to assess whether inquiries reinforced or contradicted survey results. Descriptive statistical analyses were performed using Microsoft Excel and Statistical Analysis System (SAS) statistical software package, version 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
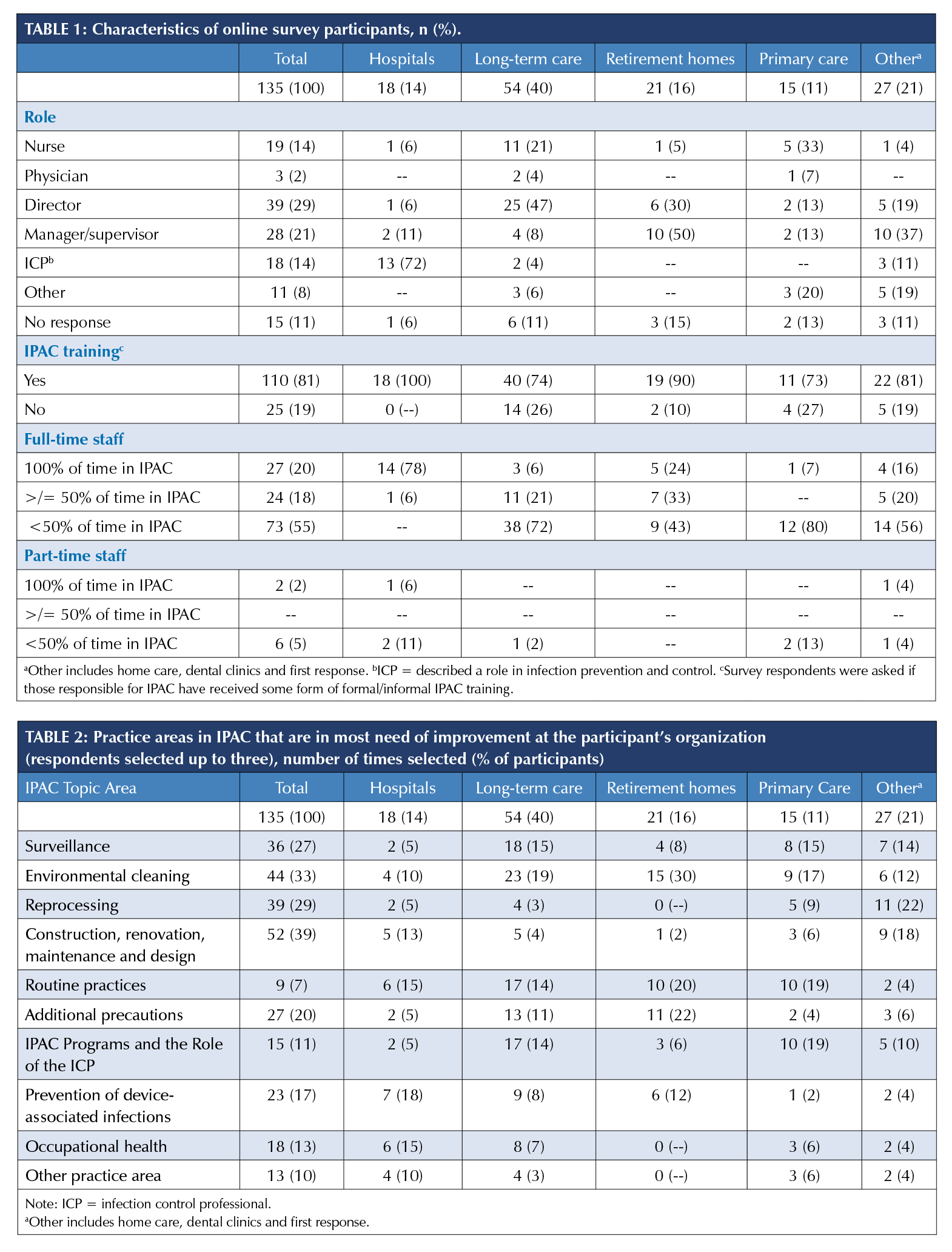
Table 1 describes the survey respondents including the settings they represent, their position, and allocation of time to IPAC related activities. The majority of respondents reported they worked in the long-term care and retirement homes.
The majority of survey respondents indicated that those responsible for IPAC have received some form of formal or informal IPAC training (81%) (Table 1). The rate of any training was highest in hospitals (100%) and lowest in primary care (73%) and long-term care (74%) (Table 1). The rate of formal training (e.g. post-secondary course) was highest in hospitals (83%), whereas other sectors were much more likely to have trained using informal resources (e.g. PHO online modules). Only 9% of respondents from non-hospital sectors reported formal training.
Areas for Improvement
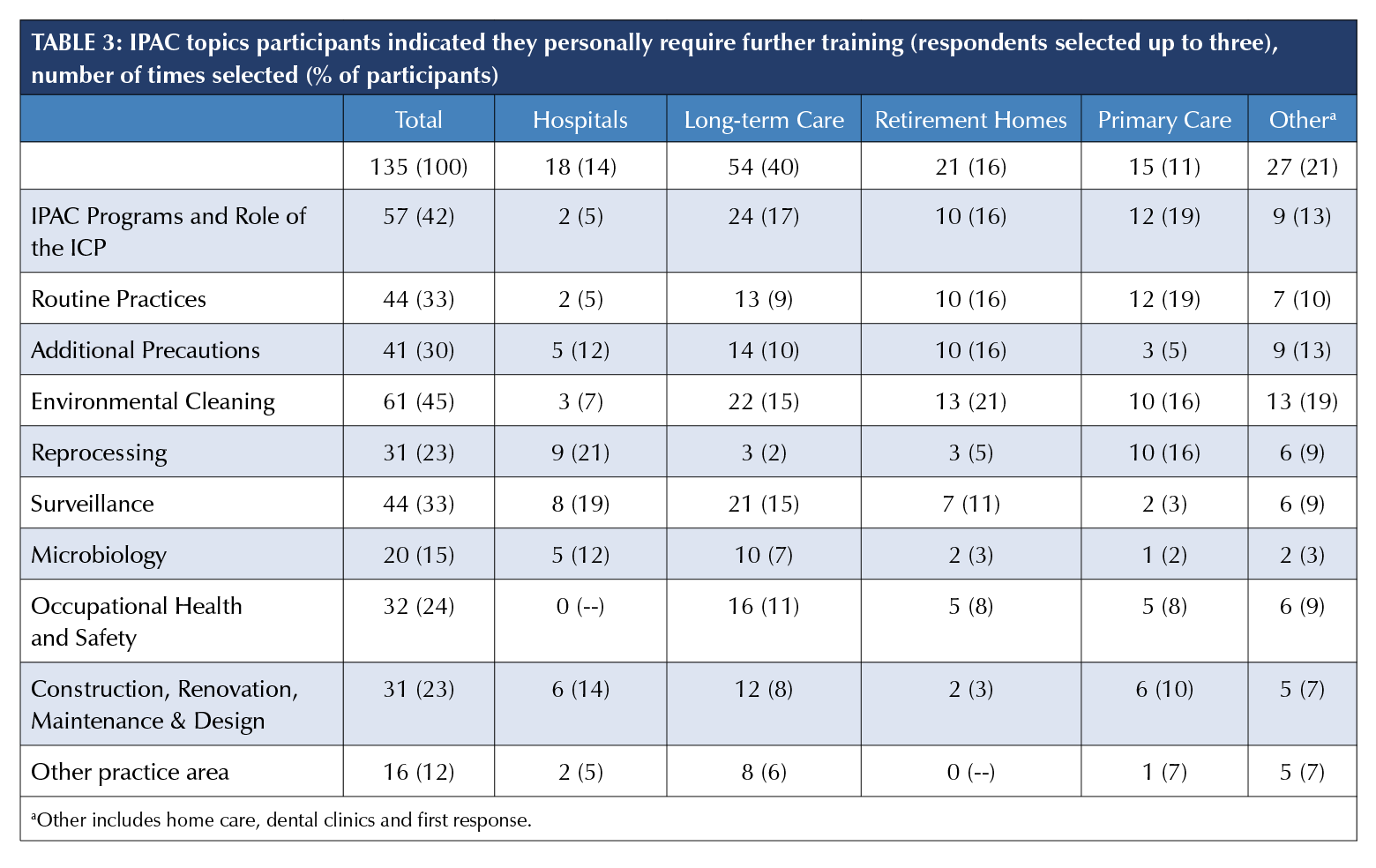
Survey respondents were asked to select up to three practice areas in IPAC that are in the most need of improvement in their organization. Results varied by setting, with environmental cleaning (42%) and routine practices (33%) dominating (Table 2).
Table 2 also shares the top three areas for each setting. There were 344 inquiries sent to PHO from this region between April 1, 2017 and March 31, 2019 with 237 (69%) of these inquiries corresponding to the IPAC practice areas defined in Table 3. The majority of these inquiries were from public health (n = 121/237, 51%) followed by dental clinics (n = 54/237, 22.8%), primary care (n = 30/237, 12%), hospitals (n = 17/237, 7.2%), long-term care and retirement homes (n = 14/237, 5.9%), and home care (n = 1/237, 0.4%) (Table 4). Reprocessing was the most common topic among inquiries received from stakeholders over this two-year period (n = 141/237, 59.5%), driven by the large number of inquiries from public health units and dental settings.
Surveillance-Related Gaps
Respondents representing hospitals (n = 17) were the most likely to report admission screening with 100% reporting methicillin-resistant Staphylococcus aureus (MRSA) screening, 91% reporting vancomycin-resistant Enterococci (VRE) screening, and 41% reporting cabapenemase-producing Enterobacteriaceae (CPE) screening. A majority of LTCH respondents (n= 54) reported that they conduct admission screening for MRSA (93%), and VRE (78%). Only two percent of long-term care homes and retirement homes reported admission screening for CPE, and only 11% and 14% respectively reported ongoing screening during admission. Inquiries regarding antibiotic resistant organisms were among the most frequent topics posed to PHO from hospitals, long-term care homes, retirement homes, and dental settings.
Reprocessing-Related Gaps
Fifty-three percent of survey respondents (n=133) indicated that their facility reprocesses medical devices and among this group, 25% reported staff at their facility are certified in reprocessing through the Medical Device Reprocessing Association of Ontario (MDRAO) or Canadian Standards Association (CSA). A large proportion of respondents indicated that they did not know whether or not a staff member was certified in reprocessing (37%). The highest rate of certification was in hospitals (n = 18, 72%). Just over half the respondents from retirement homes indicated that their facility reprocesses medical devices (n = 11, 52%); however, no respondents from retirement homes reported staff at their facility are certified.
Personal IPAC Improvement Needs
Survey respondents indicated up to three areas where they personally require improved knowledge and skills and this varied by sector (Table 3). The top four topics that were most selected for additional training across all stakeholder categories included: environmental cleaning (45%); IPAC programs and role of the ICP (42%); routine practices (33%); and surveillance (33%) (Table 3).
Hospital responses differed the most from other sectors. The top selections by hospital respondents included reprocessing (21%), surveillance (19%), and construction, renovation, maintenance and design (CRMD) (19%) (Table 3).
In all other sectors, environmental cleaning (45%); and IPAC programs and role of the ICP (42%) were the top three selections by respondents.
Requested Resources
Survey respondents were asked an open-ended question
about what additional resources could be offered to better support IPAC practices. There were a number of diverse responses that varied by healthcare setting. For example, respondents in hospital settings made note of guidelines for construction and renovation, updated Provincial Infectious Diseases Advisory Committee (PIDAC) guidelines, in addition to shorter learning modules on routine practices or additional precautions for front-line staff. In long-term care, there was an empahsis on the needs for resources on antimicrobial-resistant organisms that could be shared with residents and families in addition to simplified surveillance tools. One participant indicated a need for an online certification training for registered nurses in long-term care homes who have infection control responsibilities. There were 16 survey respondents (12%) that provided comments suggesting that they do not need additional resources.
Non-IPAC Specific Knowledge and Skill Needs
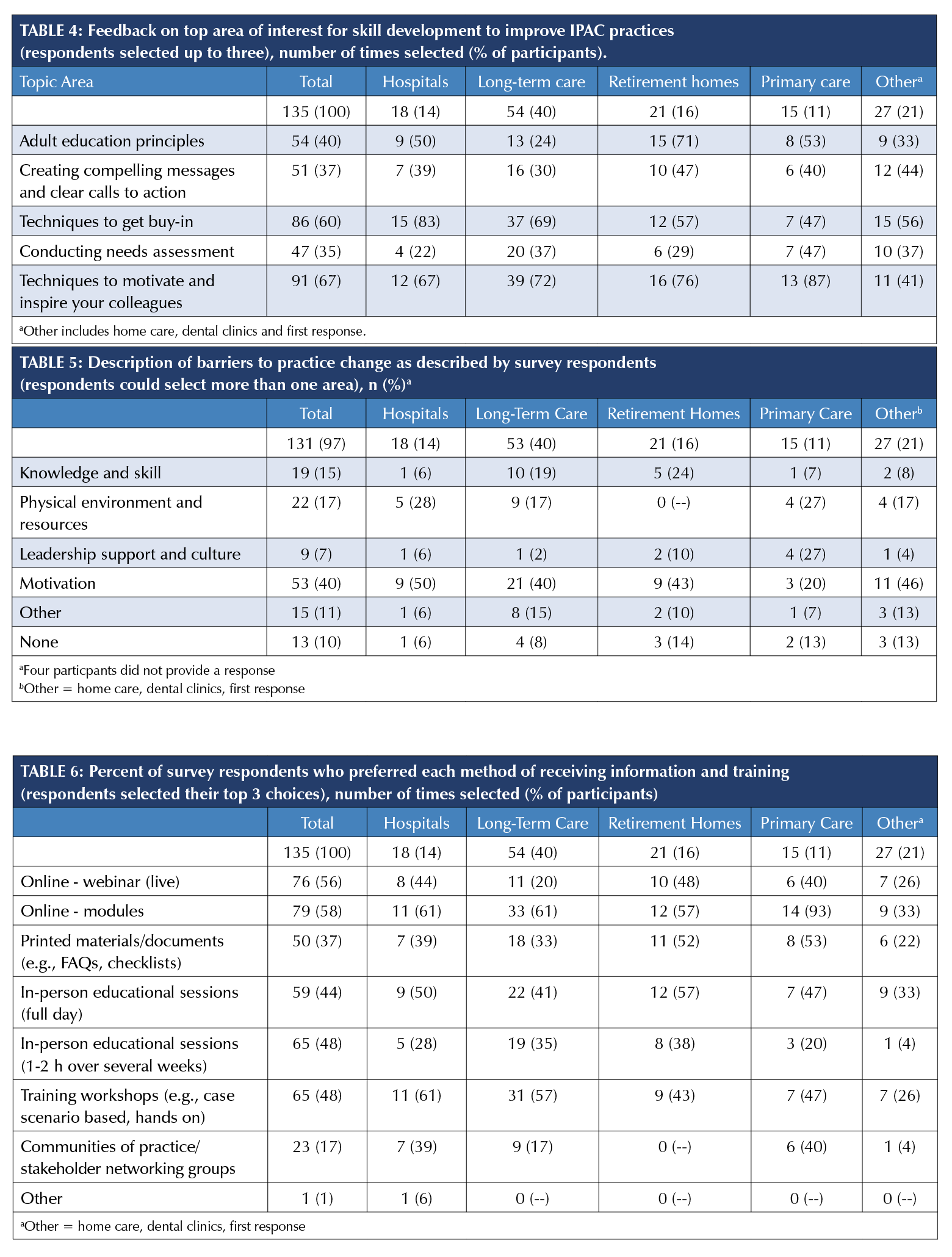
Survey respondents were asked to share levels of interest in further non-IPAC specific skill development aligning with different aspects of behaviour change. Table 4 presents an overview of levels of interest in each skill. The majority of survey respondents were interested in offerings on techniques to motivate and inspire colleagues (67%) and techniques to get buy-in (60%) (Table 4).
Barriers Influencing Practice Change or Improvement
Survey respondents highlighted motivation as the most common barrier to practice change in their organization (40%) (Table 5). There were also over 100 open-text comments about barriers to practice change. The majority of the open-text comments were barriers related to opportunity; specifically, the physical environment and resources, and motivation. Barriers that were about motivation to improve IPAC practices focused on buy-in
or risk perception. For example, a respondent noted:
“old habits die hard. When practice has been consistently below average with no serious outcomes, it is challenging to change perception and behavior.” Barriers that were related to the physical environment and resources focused on access to supplies or the age of buildings. For example, one respondent noted: “[We are dealing with an] old building, shared common resident areas, shared resident washrooms. Less than ideal hand washing stations.” There were a number of interesting reflections on the importance of leadership support and culture. For example, one responded noted: “Most managers and staff do not understand the importance and impact of IPAC. If the managers don’t understand they are not directing their
staff properly.”
Preferences for Learning Format
Survey respondents identified their preferences for receiving IPAC information and training (Table 6). Overall, for survey respondents, online modules (58%) were the most commonly selected, followed by online webinars (56%) (Table 6). Sixty-one percent of respondents working in hospitals and 63% of respondents working in long-term care selected in-person options as their first choice.
DISCUSSION
A needs assessment was conducted to prioritize future supports for IPAC professionals working across different sectors. The needs assessment provided information that will be used to prioritize areas of focus for future initiatives. The needs assessment strongly supports the importance of tailoring supports, as the results demonstrated that practice gaps, barriers to change, and preferences for learning vary across sectors.
Areas where hospital participants identified a personal need for increased knowledge and skill differed the most from other sectors. The top areas for hospital respondents included reprocessing, CRMD, and surveillance. These may be considered more advanced IPAC skills. As was identified in the needs assessment, hospitals have higher rates of full-time, formally trained IPAC employees than other sectors, and therefore, tend to have more established and longer running programs. IPAC programs and role of the ICP, and environmental cleaning were top selections by respondents from non-hospital sectors. IPAC professionals working in non-hospital sectors may benefit from further training and supports on more foundational areas of IPAC.
There were a substantial number of inquiries related to reprocessing answered by PHO over the two-year observation period, and the survey identified that a large number of facilities do not have staff certified in reprocessing. This highlights an opportunity to disseminate information about available supports and the benefits of having staff certified in reprocessing.
Although best practice guidelines [11,12] identify that LTCHs should be conducting surveillance for CPE, only 2% of LTCHs are doing so. Further investigation should be done to identify why LTCHs are not initiating screening protocols for CPE. Further investigation into the barriers will help identify approaches to improve these practices.
Across all sectors, stakeholders face barriers to practice improvement that are related to motivation. There is a strong interest in further skill development around techniques to motivate and inspire colleagues and to secure buy-in from leadership. Stakeholders may benefit from support in this area, which focuses on identifying the specific motivational barriers that are contributing to practice gaps, and strategies that can be used to overcome these.
There were both similarities and differences in preferences for learning formats across sectors, indicating a need to target teaching and information sharing by sector. Online modules and webinars were rated highly by most sectors. Online modules may be preferred as they provide a learning opportunity that can be completed at any time, while webinars provide an opportunity for posing questions, and can be done at any computer. Communities of practice/stakeholder networking groups were rated low by most sectors. Primary care respondents rated communities of practice (CoP) higher than other sectors, which may indicate fewer other opportunities to connect with colleagues across the province, as CoPs provide a venue for IPAC colleagues to network and discuss common interests.
There are a few limitations related to the distribution methods for the survey and overall response rate. There are important stakeholder groups that were not represented well by the survey including the dental setting, and the results are heavily weighted on respondents from long-term care. Given a fairly low response rate overall, those who did respond may be more likely to feel that supports in IPAC are lacking, than those who did not respond. For questions related to organizational practices, it is also important to note that the use of multiple methods to distribute the open survey could have resulted in more than one participant per organization.
It is important to take into consideration the potential for response bias in the use of an online surveys particularly when asking questions that apply to facility-level practices. There were several close-ended questions in this survey to help respondents overcome recall bias; however, there were free text options to ensure options were not missed and to encourage additional ideas.
As the survey only included participants in a particular geographical region, the results may not be applicable beyond this region. However, this region includes both rural areas and highly populated urban settings, and crosses seven public health units, which may create results that have some applicability beyond the region.
At the time of this report, there has been a significant rise in requests for support from PHO related to both foundational IPAC practices and requirements specific to the management of COVID-19. Although these topics have taken priority over the last year, the priorities identified within this needs assessment will still need to be addressed in the future. What the
COVID-19 pandemic has also exposed, and what is in alignment with the findings, is that non-hospital sectors have less advanced IPAC programs and there is a significant need for support in long-term care and primary care. The primary care response rate was very low, potentially indicating a lack of engagement in IPAC. However, the COVID-19 pandemic saw a drastic increase in inquiries and support requests from primary care settings, potentially indicating an increasing understanding of the importance of IPAC, and identifying a lack of current IPAC supports and resources in this settings. Further work must be conducted to better understand the current capacity of IPAC programs in primary care settings. The COVID-19 pandemic has also highlighted the importance of the physical environment and resource-related barriers to the successful implementation of best practices, such as the ability to physical distance, which only 17% of respondents indicated as a barrier within their facility prior to COVID-19.
Despite these limitations, this needs assessment provided an opportunity to expand connections with IPAC professionals in this region, helped identify priority areas to further explore, and also challenged assumptions about the needs of IPAC stakeholders in this region. The results of this needs assessment will be used to plan initiatives in the surveyed region and to inform initiative planning in other regions where PHO provides support.
REFERENCES
1. Graham, I.D., Logan, J., Harrison, M.B., Straus, S.E., Tetroe, J., Caswell, W., Robinson, N. (2006). Lost in knowledge translation: Time for a map? J Contin Educ Health Prof, 26(1), 13-24. https://onlinelibrary.wiley.com/doi/pdf/10.1002/chp.47
2. Field, B., Booth, A., Ilott, I., et al. (2014). Using the Knowledge to Action Framework in practice: a citation analysis and systematic review. Implementation Sc, 9, 172. https://doi.org/10.1186/s13012-014-0172-2
3. Shah, N., Castro-Sanchez, E., Charani, E., Drumright, L.N., Holmes, A.H. (2015). Towards changing healthcare workers’ behaviour: a qualitative study exploring non-compliance through appraisals of infection prevention and control practices, Journal of Hospital Infection, 90(2), 126-134. https://doi.org/10.1016/j.jhin.2015.01.023
4. Edwards, R., Charani E., et al. (2012). Optimisation of infection prevention and control in acute healthcare by use of behaviour change: a systematic review. The Lancet Infectious Diseases, 12(4), 318-329. DOI: 10.1016/S1473-3099(11)70283-3
5. Atkins, L. (2015). Using the Behaviour Change Wheel in infection prevention and control practice. Journal of Infection Prevention, 17(2). doi: 10.1177/1757177415615952
6. Gravel, D., Gardam, M., Taylor, G., et al. (2009). Infection control practices related to Clostridium difficile infection in acute care hospitals in Canada. American Journal of Infection Control, 37(1), 9-14.
7. Cadieux, G., Bhatnagar, A., Schindeler, T., et al. (2009). Assessment of the infection prevention and control learning needs of Ottawa community-based healthcare providers. Canadian Journal of Infection Control, 34(3), 135-140.
8. Zoutman, D., Douglas, B., Bryce, E., et al. (2003). The state of infection surveillance and control in Canadian acute care hospitals. Canadian Journal of Infection Control, 31(5), 266-273.
9. Infection Prevention and Control Canada. (2020). Retrieved from: https://ipac-canada.org/.
10. Michie, S., Atkins, L., West, R. (2014). The behaviour change wheel: a guide to designing interventions. London, UK: Silverback Publishing. https://doi.org/10.1186/1748-5908-6-42


