Abubaker M. Hamed PhD1, Donna Moralejo PhD, RN1, April Pike PhD, RN1, Vernon Curran PhD2
1 Faculty of Nursing, Memorial University of Newfoundland, Canada
2Faculty of Medicine, Memorial University of Newfoundland, Canada
Corresponding author:
Abubaker M. Hamed PhD
Faculty of Nursing
Memorial University of Newfoundland
Canada
Tel: 1-709-986-9410 | Email: amh040@mun.ca
ABSTRACT
Background: High nursing workload, negative role models, and inconvenient location of alcohol-based hand-rub dispensers are among the most common barriers that prevent nursing students and nurses from adhering to Routine Practices (RP). The aim of this study was to identify if nursing students and instructors encountered these three barriers, what strategies they used to address them, and how confident they were about applying problem solving in addressing them.
Method: A cross-sectional survey was conducted in three nursing schools in Eastern Canada, and included 577 undergraduate nursing students, and 20 nursing instructors. Data were collected using the Routine Practices Problem-Solving Questionnaire. Frequency distributions were used to describe the participants’ characteristics and each item in the questionnaire. Pearson chi-square test was used to assess relationships between the level of confidence and participants’ characteristics.
Results: We found that only 25% to 44.2% of students and instructors reported that high nursing workload, negative role models, and inconvenient location of alcohol-based hand rub were among the most common barriers which prevented them from adhering to Routine Practices. Although they encountered these three barriers, only 21.1% to 30.2% of students indicated that they used problem solving to address them. However, both groups of participants identified other strategies that can be used to address these three barriers. More instructors, compared to students, were very confident/confident about applying problem solving to address these barriers. There was a significant association between nursing students’ levels of confidence and their training in RP as well as their training in problem solving related to RP (p< .0001), but no significant association between the instructors’ level of confidence and these characteristics (p > 0.05).
Conclusion: Understanding of these three barriers, and knowing possible strategies to address them, including problem solving, can potentially help infection control practitioners in their discussions with nurses, students, and instructors to improve adherence to RP.
KEYWORDS: Routine infection control practices, nursing students, nursing instructors, barriers, strategies, problem solving, and confidence
INTRODUCTION
Numerous studies have shown that nursing students and nurses encounter a number of barriers which prevent them from adhering to Routine Practices (RP) such as hand hygiene, use of personal protective equipment (PPE), and sharps safety, known elsewhere as Standard Precautions (SP) [1-16]. The top three commonly reported barriers to adherence to RP in most of these studies were high nursing workload, presence of negative role models, and inconvenient location of sinks and alcohol-based hand rub (ABHR) dispensers. Encountering these barriers could lead to suboptimal adherence to RP among both nursing students and nurses. This lack of adherence may lead to increased spread of microorganisms and thus increased healthcare-associated infections (HAIs) and their negative consequences [17- 23]. Fortunately, the majority of HAIs and their negative consequences can be prevented if nursing students and nurses are able to overcome these barriers and continuously adhere to RP. To overcome these barriers, nursing students and nurses need to be equipped with some strategies which they can use, such as problem solving. Problem solving (PS) is the ability of an individual to find a solution for an issue of concern [24]. Having problem-solving skills may help students and nurses manage the complexity of today’s nursing care, including these barriers to RP adherence. However, while numerous studies have focused on various aspects of the barriers to adherence to RP, none of them has specifically focused on strategies or confidence in using PS as an approach in addressing these barriers.
Therefore, the aim of this study was to determine if nursing students and instructors encounter these three common barriers, what strategies they used to address them, and their level of confidence in using PS. Identifying these barriers and strategies, which can be used to address them, could enhance the ability of infection control practitioners (ICPs) and nurse educators, to teach and reinforce routine infection control practices when they are interacting with students and others in clinical areas.
METHOD
A cross-sectional survey was conducted in 2019 in three nursing schools in Eastern Canada: Memorial University Faculty of Nursing (MUNFON), Centre for Nursing Studies (CNS), and Western Region School of Nursing (WRSON). A total number of 577 students from Years 1-4, and 20 full-time nursing instructors were recruited in the study. The Routine Practices Problem-Solving Questionnaire (RPPSQ) was used to collect data from study participants. It was developed by the researchers based on the literature and the objectives of this study. In addition to questions about participant characteristics, they were provided with a list of potential barriers and asked to identify which barriers had prevented them from adhering to RP. The questionnaire consisted of three short-answer questions about strategies that have been used by the participant to address the three barriers of interest. There were also three items to measure participants’ confidence about applying PS to address the three identified barriers to RP adherence. The three items were scored on a 4-point Likert scale from 0 (Not at all confident) to 3 (Very confident). The total score ranged from 0-9. We then categorized level of confidence as
low if the score was ≤ 4, and high level if the score was ≥ 5. The instructors’ version differed only in phrasing. Students were asked about their own confidence, while instructors were asked about their confidence in helping students.
Prior to use in the survey, content validity of the questionnaire was established by obtaining feedback from a group of experts in infection prevention and control. In addition to experts’ feedback, a pilot test was conducted with six students and two instructors to check for completion time and to ensure the ability of participants to understand the questions correctly. Based on their feedback, minor changes were made to the questionnaire. Students in Years 1-3 completed the questionnaire during designated class time, while students in Year 4 and nursing instructors completed the questionnaires online using the online Qualtrics survey platform.
Ethical approval was obtained from the Health Research Ethic Board (HREB) and the Western Health Research Review Committee. Individual approval from each school was also obtained and participation was voluntary. Descriptive statistics were used to describe the instructors’ and nursing students’ demographic characteristics such as age, gender, and years of experience. In addition, frequencies and proportions were reported for each item in the questionnaire. Chi-square was used to assess relationships between the participants’ characteristics and their level of confidence. A p-value of less than 0.05 was considered to be statistically significant. The data were analyzed with Stata statistical software version 14.0 [25].
RESULTS
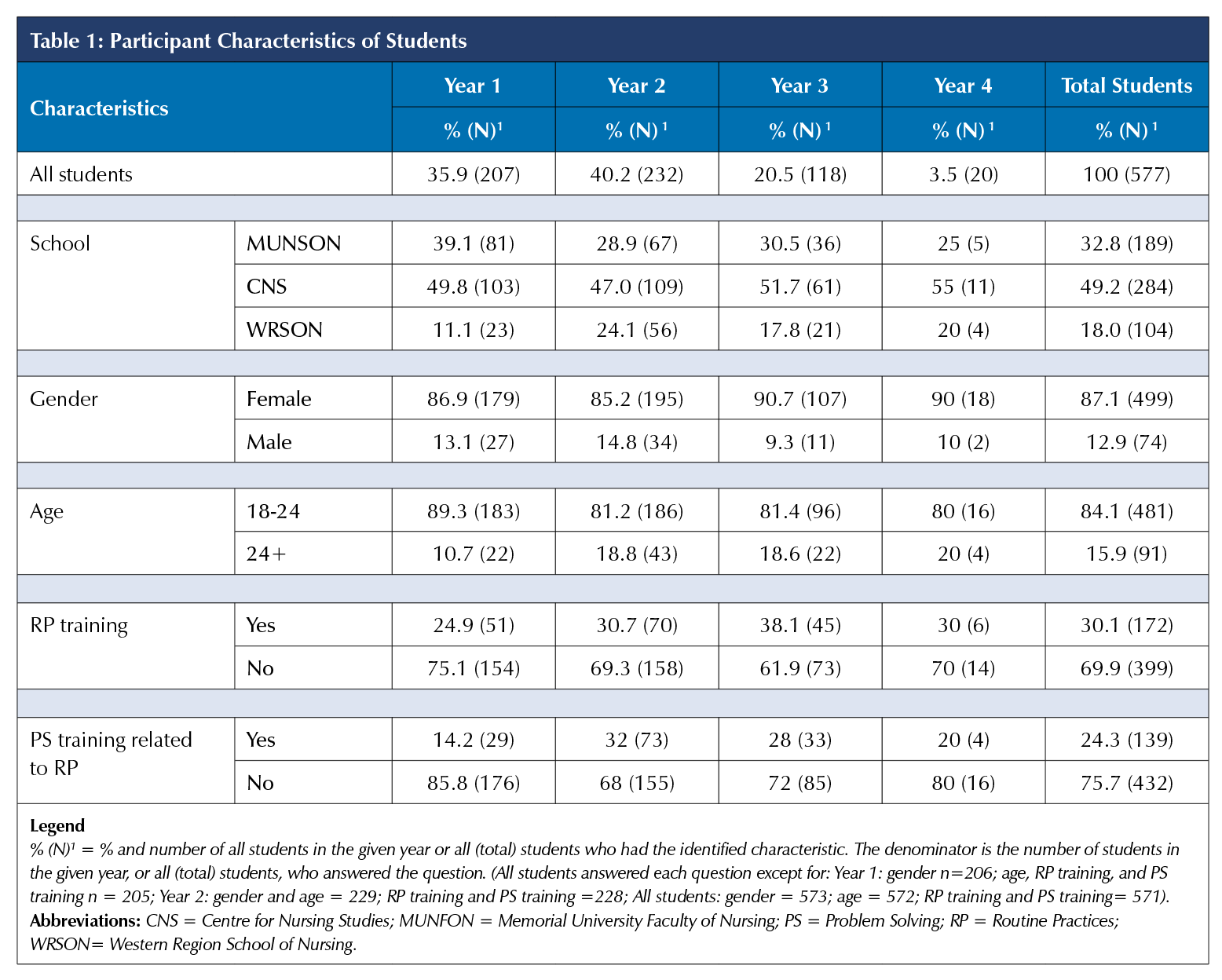
As shown in Table 1, approximately half of students (49.8%) were from the Centre for Nursing Studies, which was the largest school. There was reasonable representation for each year and school, except for Year 4, with only 20 respondents. The majority of all students were female (87.1%) and aged 18-24 (84.1%) with some variation across years. When asked if they had received additional training about RP, only 24.9% to 38.1% of the students across years reported that they had training. When asked about problem-solving training related to RP, 14.1% to 32% of the students said they had received such training. The instructors were also predominantly female (90%) with 40% from CNS, and taught in a variety of clinical settings. None of the instructors indicated that they had received extra PS training as it related to RP, and only 30% indicated that they had received extra RP training.
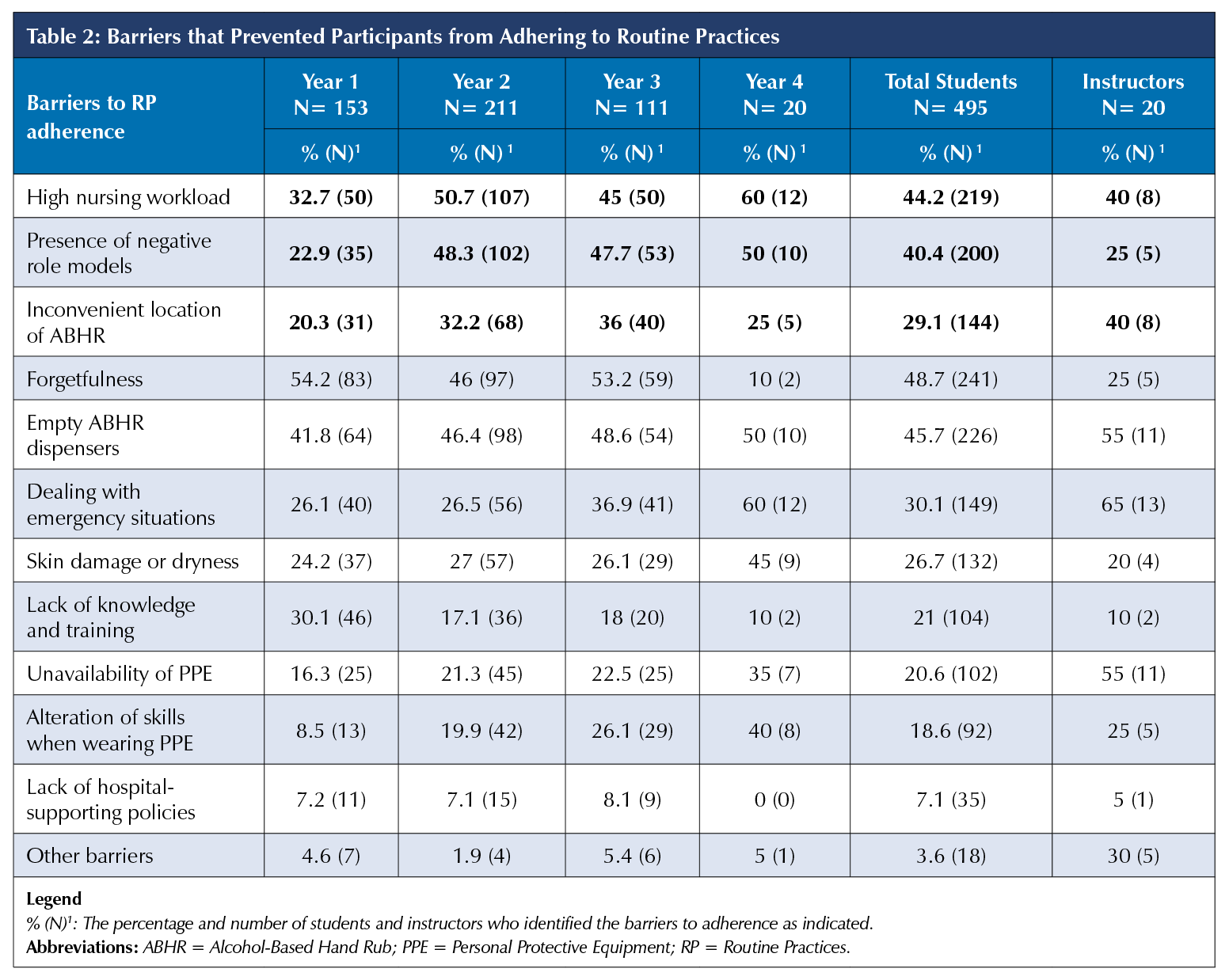
Participants were asked which barriers they had encountered, which prevented them from adhering to RP. As can be seen in Table 2, 44.2% of all nursing students, and 40% of instructors, encountered high nursing workload, 40.4% and 25% encountered negative role models, and 29.1% and 40% encountered inconvenient location of ABHR dispensers, respectively. The same three barriers were also identified by 20.3% to 60% of students across the years; a smaller proportion of students in Year 1 encountered each barrier compared to later years, likely due to less clinical experience. In addition to these three barriers, Table 2 shows that there were other barriers reported, the most common of which were forgetfulness and empty ABHR dispensers. Further analysis (not shown) found that more instructors (70% and 75%) compared to students (28.4% and 21%) reported that they used some strategies to address high nursing workload and presence of negative role models, respectively. However, only 30% in each group of participants identified some strategies that they used to address the inconvenient location of ABHR dispensers. More students in Year 4 (45% to 60%) compared to less than 40% of the students in Years 1, 2, and 3 stated that they used a strategy to address inconvenient location of ABHR and high nursing workload. However, only 15.5% to 30.2% of nursing students across all years reported strategies to address the presence of negative role models.
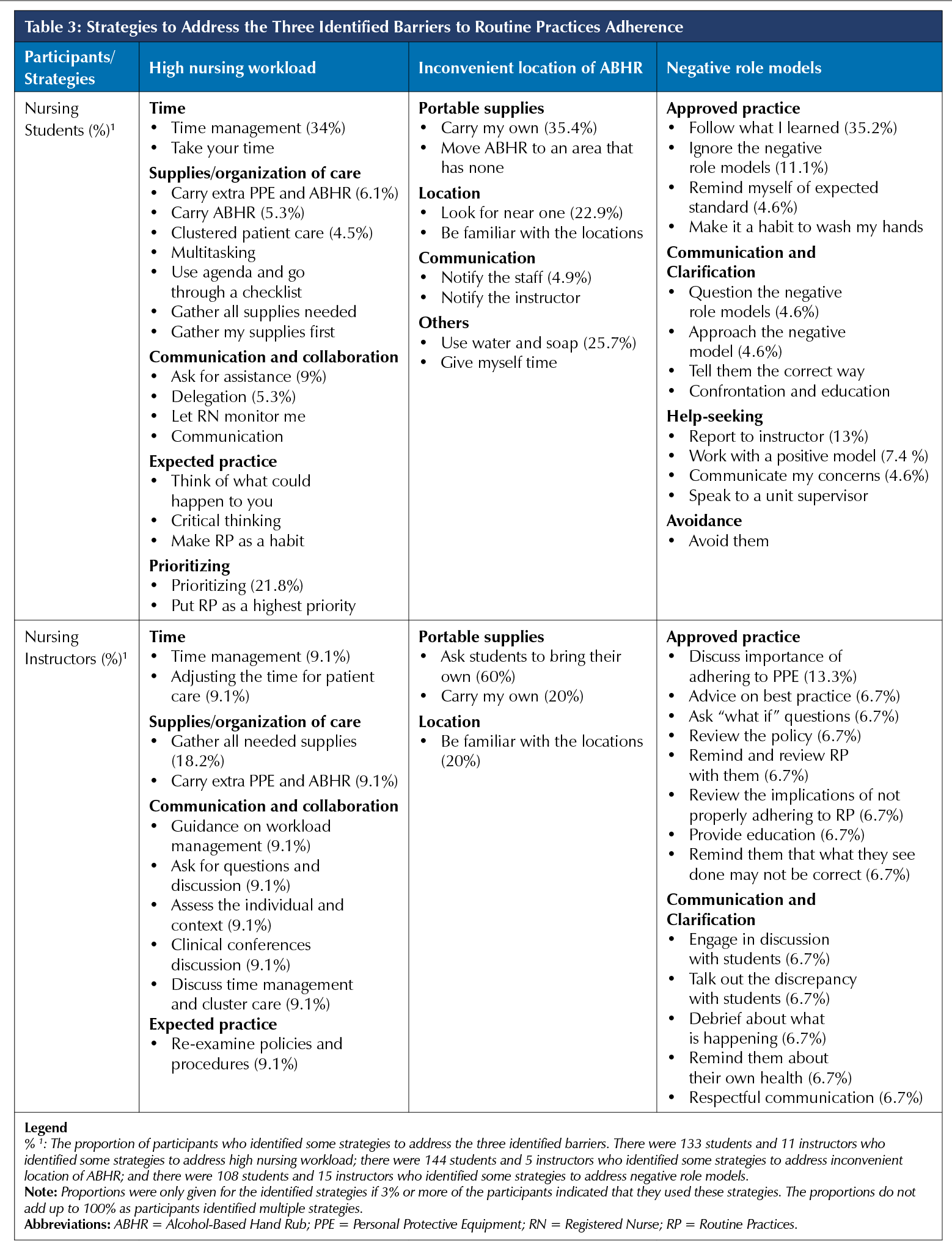
Table 3 summarizes the strategies identified by participants. There were four categories of strategies related to high nursing workload used by both students and instructors: time, supplies/organization of care, communication and collaboration, and expected practice. Students also identified strategies related to prioritizing. For example, 34% of the students and 9.1% of the instructors identified time management as a useful strategy, while gathering supplies was a strategy reported by 18.2% of the instructors, and less than 3% of the students. An example of communication and collaboration was to ask for assistance, while a few answers related to expectations, e.g., “make RP a habit”. To address the inconvenient location of ABHR, portable supply and location were the two key categories of strategies identified, with 35.4% of the students and 20% of the instructors identifying “carry my own”. However, to address negative role models, strategies related to approved practice, communication and clarification were identified by both groups; students also identified strategies related to help-seeking and avoidance. For instance, the most common ones identified by students were “follow what I learned” (35.2%) and “report to the instructor” (13%), while the instructors identified “discuss importance of adhering to PPE” (13.3%).
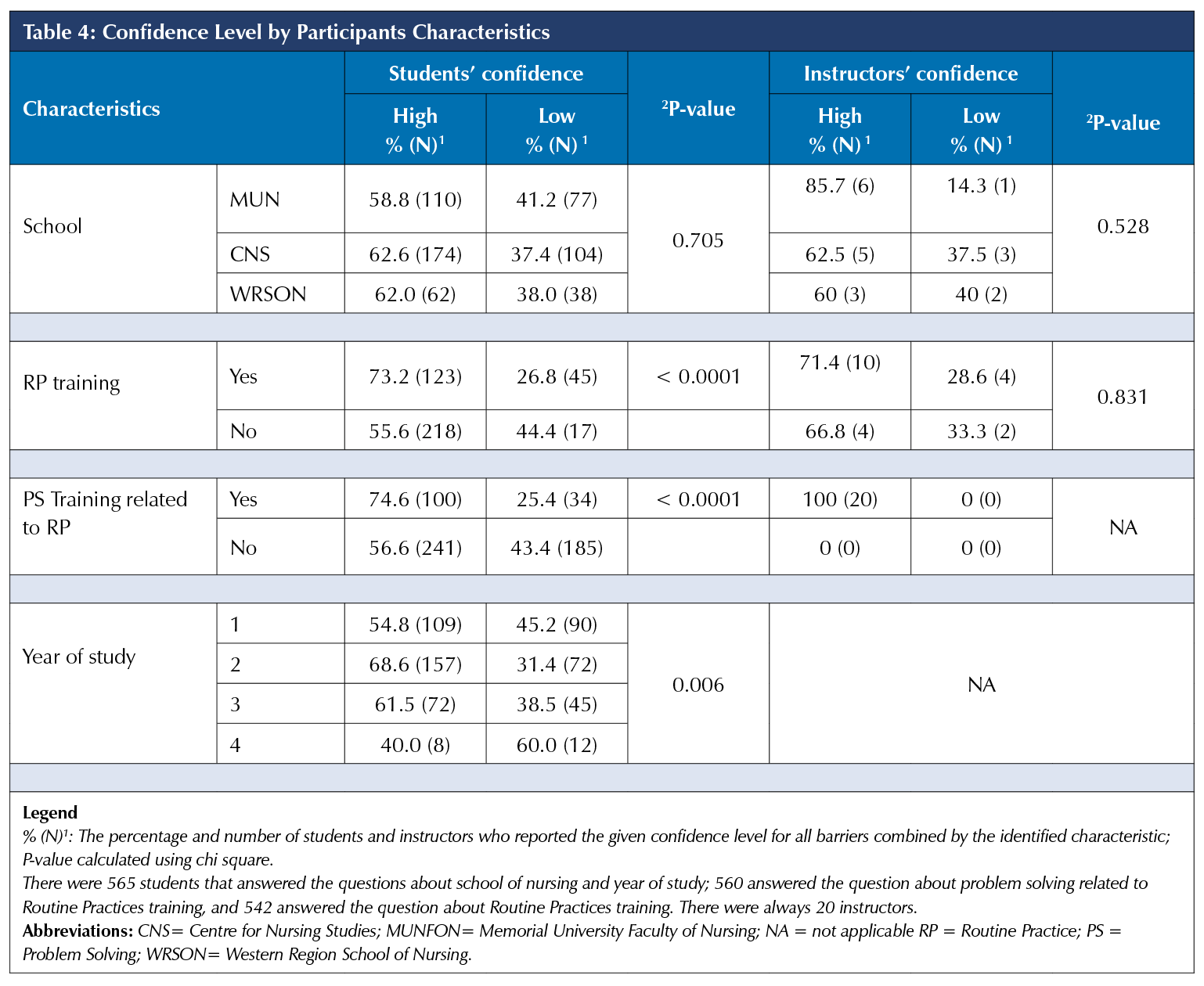
Overall, 61.2% of students and 70% of the instructors were categorized by their scores as having high confidence in addressing the three barriers of interest. Chi-square tests showed a significant relationship between nursing students’ level of confidence and their training about RP and training about PS related to RP (p < .0001). However, there were no significant differences in confidence by their year of study (p = 0.010), age (p = 0.178), and gender (p = 0.080). A lower proportion of students in Year 4 (40%) had high confidence compared to other years and this difference was statistically significant (p = 0.006). However, there was no significant relationship between the instructors’ characteristics and their level of confidence (p < 0.05).
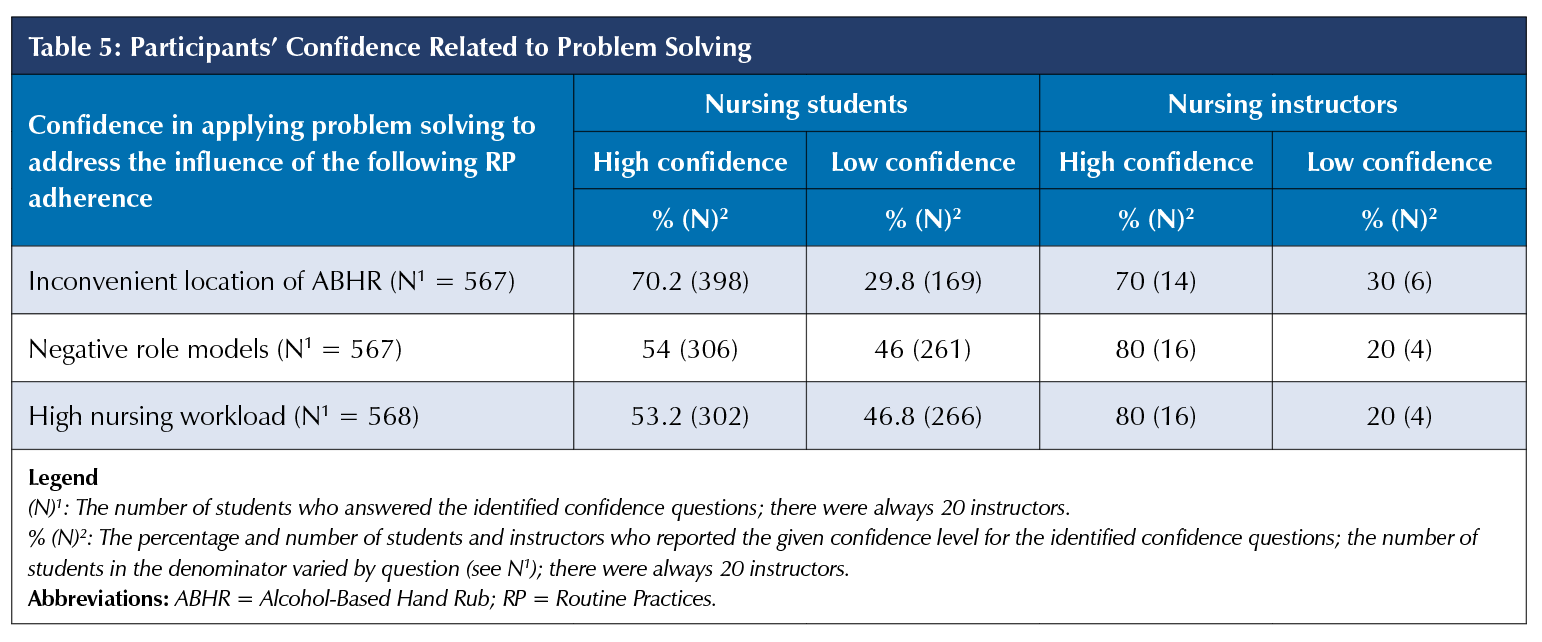
As shown in Table 5, instructors showed a high level of confidence (80% and 80%) compared to students (53.2% and 54%) about applying PS to address high nursing workload and negative role models, respectively. However, 70% of each group of participants showed a high level of confidence in applying PS to address the inconvenient location of ABHR dispensers.
DISCUSSION
For the purpose of this study, we defined high nursing workload as busyness, too many tasks to perform, and lack of time to perform nursing care, while a negative role model was defined as a nurse who does not frequently or appropriately adhere to RP. However, these terms were not defined to participants, and they answered questions based on their own understanding. Both groups of participants reported a number of barriers that prevented them from adhering to RP. However, in this study, we focused our discussion on the top three commonly reported barriers to adherence to RP in most of the reviewed studies, as well as in this study. The three most commonly encountered barriers were high nursing workload, presence of negative role models, and inconvenient location of ABHR dispensers.
High nursing workload
This study found that 44.2% of nursing students and 40% of nursing instructors reported that high nursing workload was one of the common barriers that prevented them from adhering to RP. The results of our study are similar to the findings documented in previous studies, where 44% of Ghanaian nursing students [1]
and 26% of Indian students [12] reported that they did not have enough time to adhere to Standard Precautions (SP). Moreover, studies conducted in Canada and in China also found that 23% and 35% of nursing students, respectively, reported that “busyness” influenced their adherence to SP [3,7].
Busyness and lack of time could be attributed to a high nursing workload. Our study findings are also comparable to a study in the United Kingdom, where 59.9% of nursing students reported that high workload was one of the key factors that influenced their adherence to infection prevention and control practices [8]. Similar results for both nurses and nursing students were also obtained by five qualitative research studies, in which lack of time, very busy schedules, and too many tasks and patients to care for were among the main barriers which prevented them from adhering to infection prevention and control practices [2, 9, 13, 14, 26].
Although both groups of participants reported that high nursing workloads was one of the barriers which influenced their adherence to RP, this study found that fewer students (28.4%), compared to instructors (70%), identified some unique strategies that they used to address this barrier. These unique strategies were categorized into four categories: time, supplies/organization of care, communication and collaboration, and expected practice. Under each of these four categories, both students and instructors identified a number of strategies. However, the common strategies were time management, prioritizing, and gathering all needed supplies. To our knowledge, this study is the first to identify these strategies. Therefore, there were no studies in the literature for comparison.
Presence of negative role models
Our results showed that more students (40.4%) compared to instructors (25%) experienced the issue of negative role models in their clinical practice. This study finding is consistent with findings from other studies. For example, Wilson et al. (2017) found that 38% of nursing students self-reported that the presence of negative role models affected their adherence to infection prevention and control practices [15]. Similar to our result, one study conducted in a university in Hong Kong by Cheung et al. (2015) found that second- and third-year nursing students’ adherence to SP was significantly influenced by the adherence of other nurses in the unit [3]. A more recent study among 350 nursing students from eight universities in Korea found that the intention of nursing students to adhere to infection prevention and control practices was negatively influenced by the non-adherence of other nurses in their clinical settings [4]. Furthermore, in two qualitative research studies on the barriers to SP adherence, nursing students stated that the presence of negative role models was one of the main factors that prevented them from adhering to SP [9, 14].
Despite the impact that negative role models may have on the participants’ adherence to RP, only 21% of students stated that they used some strategies to address it. To address the issue of negative role models, both groups of participants identified a number of strategies which they used. We have also categorized them into four categories of strategies for the students (approved practice, communication and clarification, help-seeking, and avoidance) and two categories of strategies for the instructors (approved practice and communication and clarification). However, the most commonly identified strategies in these categories by both groups were: “follow what I learned”, “report to instructor”, “discuss importance of adhering to PPE”, and “ignore the negative role models”.
Inconvenient location of ABHR dispensers
According to our study findings, 29.1% of the students and 40% of the instructors reported that this barrier prevented them from adhering to hand hygiene. This result is consistent with findings from a number of studies. For instance, the authors of two Canadian studies explored the perceived predictors of hand hygiene and found that 36% of nursing students and 41% of nurses indicated that the inconvenient location of ABHR dispensers and handwash sinks was one of the barriers that prevented them from adhering to hand hygiene [7, 10]. Besides the inconvenient location, visibility of ABHR dispensers and sinks can also influence adherence to hand hygiene. For instance, nurses and other healthcare workers (HCWs) were more likely to adhere to hand hygiene if ABHR dispensers and sinks were in more visible locations [5, 16]. Moreover, nurses were significantly more likely to adhere to hand hygiene if handwash sinks were in their direct line of vision, compared to those who did not visualize these sinks (p = 0.001) [5]. Similarly, after two new sinks were placed in visible locations, hand hygiene adherence of nursing staff and other HCWs was significantly increased from 33.8% to 51.6% (p = 0.03), and the number of HCWs who did not clean their hands was significantly decreased from 54% to 37% (p = 0.001) [16]. Similar to our result, a recent study examined the impact of visibility of and accessibility to ABHR dispensers on adherence to hand hygiene in two nursing units. The authors of this study found that nurses who worked on the unit with visible and accessible location of ABHR dispensers had a significantly higher adherence rate to hand hygiene 5.17% (p = 0.001) compared to those who worked on the unit where ABHR dispensers were not visible or accessible (1.5%) [27].
Although both groups of participants stated that the inconvenient location of ABHR dispensers prevented them from adhering to RP, only 30% of both participants were able to identify some strategies that can be used to address it. These strategies were also placed into four categories for students (portable supplies, location, communication, and others) and two categories for the instructors (portable supplies and location). The common strategies identified by both groups of participants were: “carry my own” (35.4%), “look for near one” (22.9%), “students bring their own” (60%), and “be familiar with the locations of ABHR dispensers” (20%). It is not possible to compare our findings about these strategies to the literature as to the best of our knowledge, no studies have addressed strategies used by nurses or students.
Other barriers
Besides the three barriers just discussed, our study results also showed that both groups of participants also reported other common barriers which prevented them from adhering to RP. These barriers included forgetfulness, empty ABHR dispensers, dealing with emergency situations, and unavailability of PPE. Similar findings were reported in other studies [3, 4, 6, 7, 8, 10, 15]. These barriers, however, were not explored in more detail in this study.
Confidence using problem solving to address the three barriers
Considering the majority of students (80%) and instructors (75.7%) stated that they did not have PS training for RP, it is surprising that 70% to 80% of the instructors and 53.2% to 70.2% of students were very confident/confident about applying PS to address the inconvenient location of ABHR, negative role models, and high nursing workload, although more instructors had these levels of confidence. Our findings contradicted the results of an earlier study conducted in Atlantic Canada which found that only 26.9% of nursing educators and 20.0% of nursing students reported feeling very confident in PS related to infection prevention and control [28]. This contradiction could be because that researcher assessed PS related to infection prevention and control in general, and we specifically assessed PS related to the three barriers. It could be also due to a response bias, as participants in our study may have overestimated their confidence about using PS to address these three barriers.
Confidence in using PS to address the barriers was significantly associated with additional training in both RP and PS related to RP. It was not possible to assess the actual impact of the training in this study, but the results suggest that further evaluation of PS training is warranted. It was also interesting to find that a significantly smaller proportion of Year 4 students (40%) compared to Years 1-3 students (54.8%-68.8%) were confident about PS related to the barriers. This may be an artifact of the small sample of Year 4 students, but future research can explore the need for additional PS training in senior students, e.g., as a refresher.
Implications for infection control practitioners
As previously discussed, these three barriers could have a negative impact on students’ and nurses’ adherence to RP. Although the study focused on students and instructors, the results can also be useful in informing discussions with practicing nurses. Therefore, it is important for ICPs to be familiar with the strategies to address these three barriers, so that they can reinforce their application in clinical practice. For example, to address high nursing workload, ICPs can discuss how planning for sufficient time to perform hand hygiene or use PPE, or how gathering key supplies so the nurse or student does not have to leave the bedside and return, can help them incorporate RP into practice and make provision of care more efficient.
Awareness of these strategies can also help ICPs in their discussions with students and nurses when negative role models are known or suspected to be an influence on their adherence to RP. Awareness and discussion of these strategies can be a starting point for exploring how the individual could follow what they learned, and ignore the negative role model, or how reporting it can help nursing students to address the problem and have better adherence to RP. In addition, ICPs can also use their communication skills to discuss the issue of negative role models with nurses, and explain to them its negative impact on the adherence to RP. Moreover, ICPs can encourage nurses and instructors to become positive role models by continuously adhering to RP when it is required.
It may not always be feasible for students and nurses to change the location of ABHR dispensers and handwash sinks, but ICPs can use their knowledge and leadership skills to participate in designing and selecting convenient locations to place ABHR dispensers and handwash sinks. More importantly, ICPs can reinforce the possibility of HCWs bringing their own ABHR, or the use of portable ABHR. These strategies can be brought out in a discussion of a point-of-care risk assessment in terms of recognizing that hand hygiene is needed, and problem-solving options are considered to ensure it is performed.
Strengths and limitations of the study
A key strength of this study is that this was the first survey study of its kind to identify strategies used and confidence to address these three barriers to RP adherence. Another strength of this study is that there was a good representative sample size of
557 students from Years 1 to 3 from three main nursing schools in Atlantic Canada. However, this study has some limitations. There was a limited number of nursing instructors and Year 4 nursing students from the three nursing schools which participated in this study. This could be due to the fact that these two groups completed the survey online. Therefore, the results may not be generalizable to other instructors and Year 4 students. In this study, we used a self-report questionnaire, therefore, we cannot exclude possible over or underestimation of participants’ confidence to address these three identified barriers. We cannot be sure that the findings about strategies used were complete and therefore could not assess the association between confidence and practice; these can be assessed in future studies. In this study, we developed our questionnaire based on the gaps in the literature and the objectives of this study. Future research could focus on the development and validation of a questionnaire to assess problem solving related to RP.
CONCLUSION
This study has highlighted that both nursing instructors and nursing students across all years encountered a number of barriers, such as high nursing workload, negative role models, and inconvenient location of ABHR dispensers, which prevented them from adhering to RP. Although they encountered these barriers, only a few of them identified some strategies that can be used to use to address them. These identified strategies were varied between the participants. Both the application of strategies and their confidence about using PS to address these barriers to RP adherence need to be strengthened. Addressing these barriers may lead to improved students’ adherence, and as a result, may also improve patient safety. Together, we think that this knowledge is relevant to ICPs as understanding of these three barriers and strategies to address them can potentially help ICPs to reinforce their approach to improve staff adherence to RP.
REFERENCES
1. Akagbo, S. E., Nortey, P., & Ackumey, M. M. (2017). Knowledge of standard precautions and barriers to compliance among healthcare workers in the Lower Manya Krobo District, Ghana. BMC Research Notes, 10(1), 432. https://doi.org/10.1186/s13104-017-2748-9
2. Atif, S., Lorcy, A., & Dubé, E. (2019). Healthcare workers’ attitudes toward hand hygiene practices: Results of a multicentre qualitative study in Quebec. Canadian Journal of Infection Control, 34(1). Available at https://ipac-canada.org/photos/custom/CJIC/CJIC_Spring2019_Atif.pdf.
3. Cheung, K., Chan, C. K., Chang, M. Y., Chu, P. H., Fung, W. F., Kwan, K. C., ... & Mak, H. M. (2015). Predictors for compliance of standard precautions among nursing students. American Journal of Infection Control, 43(7), 729-734. https://doi.org/10.1016/j.ajic.2015.03.007.
4. Choi, J. S., & Kim, K. M. (2018). Factors influencing nursing students’ intention to comply with infection control practices. American Journal of Infection Control, 46(6), 717-719. https://doi.org/10.1016/j.ajic.2017.12.010.
5. Deyneko, A., Cordeiro, F., Berlin, L., Ben-David, D., Perna, S., & Longtin, Y. (2016). Impact of sink location on hand hygiene compliance after care of patients with Clostridium difficile infection: a cross-sectional study. BMC Infectious Diseases, 16(1), 203. https://doi.org/10.1186/s12879-016-1535-x.
6. Dorgham, S. R., & Obied, H. K. (2016). Factors affecting nurse interns’ compliance with standard precautions for preventing stick injury. Journal of Nursing Education and Practice, 6(12), 121–130. https://doi.org/10.5430/jnep.v6n12p121 .
7. Foote, A., & El-Masri, M. (2016). Self-perceived hand hygiene practices among undergraduate nursing students. Journal of Research in Nursing, 21(1), 8-19. https://doi.org/10.1177/1744987115606959.
8. Hinkin, J., & Cutter, J. (2014). How do university education and clinical experience influence pre-registration nursing students’ infection control practice? A descriptive, cross-sectional survey. Nurse Education Today, 34(2), 196-201. https://doi.org/10.1016/j.nedt.2013.09.005.
9. Kim, K. M., & Oh, H. (2015). Clinical experiences as related to standard precautions compliance among nursing students: a focus group interview based on the theory of planned behavior. Asian Nursing Research, 9(2), 109-114. https://doi.org/10.1016/j.anr.2015.01.002.
10. Kirk, J., Kendall, A., Marx, J. F., Pincock, T., Young, E., Hughes, J. M., & Landers, T. (2016). Point of care hand hygiene—where’s the rub? A survey of US and Canadian health care workers’ knowledge, attitudes, and practices. American Journal of Infection Control, 44(10), 1095-1101. https://doi.org/10.1016/j.ajic.2016.03.005.
11. Quan, M., Wang, X., Wu, H., Yuan, X., Lei, D., Jiang, Z., & Li, L. (2015). Influencing factors on use of standard precautions against occupational exposures to blood and body fluids among nurses in China. International Journal of Clinical and Experimental Medicine, 8(12), 22450. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4730013/.
12. Rashmi, A., & Kundapur, R. (2017). Factors influencing observation of standard precautions among nursing staff in tertiary care setting in Mangalore. International Journal of Community Medicine and Public Health, 5(1), 377-381.
http://dx.doi.org/10.18203/2394-6040.ijcmph20175817.
13. Travers, J., Herzig, C. T., Pogorzelska-Maziarz, M., Carter, E., Cohen, C. C., Semeraro, P. K., ... & Stone, P. W. (2015). Perceived barriers to infection prevention and control for nursing home certified nursing assistants: a qualitative study. Geriatric Nursing, 36(5), 355-360. https://doi.org/10.1016/j.gerinurse.2015.05.001.
14. Ward, D. J. (2013). The barriers and motivators to learning infection control in clinical placements: interviews with midwifery students. Nurse Education Today, 33(5), 486-491. https://doi.org/10.1016/j.nedt.2012.05.024.
15. Wilson, J., Bak, A., Whitfield, A., Dunnett, A., & Loveday, H. (2017). Public perceptions of the use of gloves by healthcare workers and comparison with perceptions of student nurses. Journal of Infection Prevention, 18(3), 123-132. https://doi.org/10.1177/1757177416680442.
16. Zellmer, C., Blakney, R., Van Hoof, S., & Safdar, N. (2015). Impact of sink location on hand hygiene compliance for Clostridium difficile infection. American Journal of Infection Control, 43(4), 387-389. https://doi.org/10.1016/j.ajic.2014.12.016.
17. Arefian, H., Hagel, S., Fischer, D., Scherag, A., Brunkhorst,
F. M., Maschmann, J., & Hartmann, M. (2019). Estimating extra length of stay due to healthcare-associated infections before and after implementation of a hospital-wide infection control program. PloS One, 14(5), e0217159. https://doi.org/10.1371/journal.pone.0217159.
18. Badia, J. M., Casey, A. L., Petrosillo, N., Hudson, P. M., Mitchell, S. A., & Crosby, C. (2017). Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. Journal of Hospital Infection, 96(1), 1-15. https://doi.org/10.1016/j.jhin.2017.03.004.
19. Canadian Nosocomial Infection Surveillance Program (CNISP). (CNISP, 2015). Healthcare-associated Infections Annual Report 2009-2014. Retrieved from: https://www.health.gov.nl.ca/health/publichealth/cdc/hai/hai_2014.pdf.
20. Olsen, M. A., Yan, Y., Reske, K. A., Zilberberg, M. D., & Dubberke, E. R. (2015). Recurrent Clostridium difficile infection is associated with increased mortality. Clinical Microbiology and Infection, 21(2), 164-170. https://doi.org/10.1016/j.cmi.2014.08.017.
21. Schmidt, A., Bénard, S., & Cyr, S. (2015). Hospital cost of staphylococcal infection after cardiothoracic or orthopedic operations in France: a retrospective database analysis. Surgical Infections, 16(4), 428-435. https://doi.org/10.1089/sur.2014.045.
22. Schweizer, M. L., Cullen, J. J., Perencevich, E. N., & Sarrazin, M. S. V. (2014). Costs associated with surgical site infections in Veterans Affairs hospitals. JAMA Surgery, 149(6), 575-581. https://doi.org/10.1001/jamasurg.2013.4663 .
23. Zimlichman, E., Henderson, D., Tamir, O., Franz, C., Song, P., Yamin, C. K., ... & Bates, D. W. (2013). Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Internal Medicine, 173(22), 2039-2046. https://doi.org/10.1001/jamainternmed.2013.9763.
24. Ahmady, S., & Shahbazi, S. (2020). Impact of social problem-solving training on critical thinking and decision making of nursing students. BMC Nursing, 19(1), 1-8. https://doi.org/10.1186/s12912-020-00487-x.
25. StataCorp. (2015). Statistical Software: Release 14. College Station, TX: StataCorp LP.
26. Barker, A. K., Brown, K., Siraj, D., Ahsan, M., Sengupta, S., & Safdar, N. (2017). Barriers and facilitators to infection control at a hospital in northern India: a qualitative study. Antimicrobial Resistance & Infection Control, 6(1), 35. https://doi.org/10.1186/s13756-017-0189-9.
27. Cai, H., Tyne, I. A., Spreckelmeyer, K., & Williams, J. (2021). Impact of Visibility and Accessibility on Healthcare Workers’ Hand-Hygiene Behavior: A Comparative Case Study of Two Nursing Units in an Academic Medical Center. HERD: Health Environments Research & Design Journal, 14(2), 271-288. https://doi.org/10.1177/1937586720962506.
28. Chiasson, M. (2015). Exploring infection prevention and control education in Atlantic Canadian undergraduate nursing education programs (Doctoral dissertation, Memorial University of Newfoundland). Available at https://research.library.mun.ca/8446/.


