Reprinted with permission from University of Toronto Press (https://utpjournals.press). Official Journal of the Association of Medical Microbiology and Infectious Disease Canada 7.3, 2022 doi:10.3138/jammi-2022-08-08
Jennifer M Grant MD, CM, FRCPC,1 Justin Chan MD, MPH, FRCPC,2 Sylvain A Lother MD, DTMH, FRCPC,3 Lisa Barrett MD, PhD, FRCPC,4 Paul E Bonnar MD, FRCPC,5 Aidan R Findlater MD, MSc, FRCPC,6 Sameer S Kassim MBBChBAO, MSc, DTM&H, CCFP, DipRCPath,7 John C Lam MD, FRCPC, MSc,8 Donald C Vinh MD, FRCP(C), FCIS9
1Division of Medical Microbiology and Division of Infectious Diseases, University of British Columbia, Vancouver, British Columbia, Canada;
2Division of Infectious Diseases and Immunology, Department of Medicine, New York University Grossman School of Medicine, New York, New York, United States;
3Divisions of Critical Care and Infectious Diseases, Department of Medicine, University of Manitoba, Winnipeg, Manitoba, Canada;
4Division of Infectious Diseases, Department of Medicine, Department of Microbiology and Immunology, Queen Elizabeth II Hospital, Dalhousie University, Halifax, Nova Scotia, Canada;
5Division of Infectious Diseases, Queen Elizabeth II Hospital, Dalhousie University, Halifax, Nova Scotia, Canada;
6Division of Infectious Diseases, Department of Medicine, McMaster University, Hamilton, Ontario, Canada;
7Department of Family Medicine, University of Manitoba, Winnipeg, Manitoba;
8Division of Infectious Diseases, Department of Medicine, University of Calgary, Calgary, Alberta, Canada;
9Division of Infectious Diseases, Department of Medicine; Division of Medical Microbiology, Department of Laboratory Medicine, McGill University Health Centre, Montreal, Quebec, Canada
Corresponding author:
Jennifer M. Grant
Division of Medical Microbiology and Division of Infectious Diseases
Vancouver General Hospital, JPPN Room
1112 899 West 12th Ave
Vancouver, B.C. V5Z 1M9
Tel: 604-875-5083
This email address is being protected from spambots. You need JavaScript enabled to view it.
INTRODUCTION
The COVID-19 pandemic has generated an enormous need for effective treatments. This Practice Point provides clinicians with succinct, evidence-based guidance in the care of patients with COVID-19. The recommendations need to be considered in the context of drug availability and practicality. In the context of shortages or logistical challenges, a systematic approach is needed to ensure that patients at the highest risk for poor outcomes have equitable access based on ethical principles. Infection prevention and control measures, management of complicated or long COVID-19, recommendations in children, and vaccination are not within the scope of this document. This AMMI Canada Practice Point is intended to be a living document, informed by real-world efficacy as data emerge on new variants and therapies to ensure that contemporary evidence continues to inform clinicians in responsibly using resources to provide the best possible medical care throughout the course of the COVID-19 pandemic.
METHOD
AMMI Canada members representing all regions of the country (see authorship) undertook this Practice Point. It is based on publicly available provincial treatment guidelines and peer-reviewed literature. Consensus was reached either by concordance between published guidelines, group consensus, or majority vote. Unequivocal recommendations are noted with “recommend” or “don’t recommend,” while those treatments that remain uncertain are denoted with a “neither recommend nor discourage” designation. Important qualifiers are found in the text.
In this document, the following definitions for disease severity are used, regardless of patient location.
Mild: Patients who do not need oxygen supplementation above baseline requirements to maintain an arterial oxygen saturation of > 92%.
Moderate: Patients admitted to hospital or requiring either low-flow oxygen or an increased amount of oxygen compared to baseline (for those already on supplemental oxygen), to maintain an arterial oxygen saturation of > 92%.
Severe: Patients who require high-flow oxygen or non-invasive ventilation but not organ support.
Critical: Patients who require invasive ventilation or other organ support.
AMMI CANADA RECOMMENDATIONS
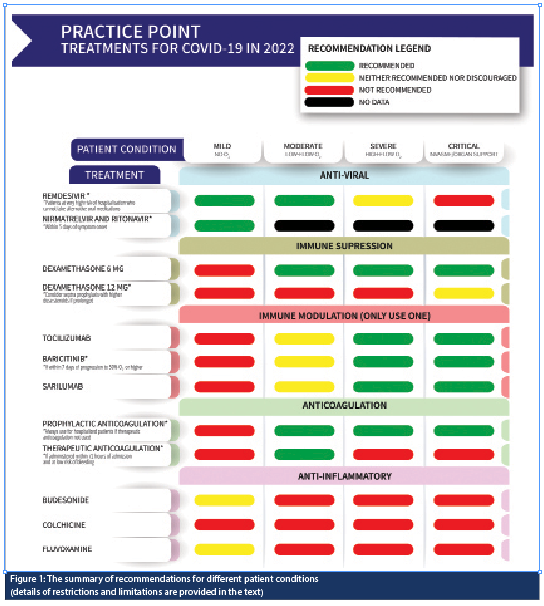
The summary of recommendations for different patient conditions are shown in Figure 1.
RECOMMENDED THERAPIES
Disease prevention
Vaccination: Vaccines are the best means of avoiding adverse outcomes from SARS-CoV-2 infection. This working group strongly encourages all Canadians to follow public health recommendations on vaccination appropriate for their age and health status.
Pharmacologic prophylaxis: There are no clinical data supporting the use of antiviral agents as post-exposure prophylaxis. There is currently one drug with data available for pre-exposure prophylaxis: cilgavimab/tixagevimab (Evusheld). The external validity of the primary study [1] to targeted populations (e.g., immune suppressed) is low. In the context of high population levels of imperfect immunity (via vaccination and illness) and less virulent viral strains, the benefits of cilgavimab/tixagevimab usage are unclear and therefore not recommended for the general population. There are insufficient data to recommend for or against cilgavimab/tixagevimab therapy for the immunocompromised.
Treatment of disease
Disease treatment is generally targeted to different physiologic systems depending on the stage of the disease. Early disease treatments are aimed at supporting immune response against the virus or directly attacking the virus. Later in the course, treatments focus primarily on addressing excessive immune responses and hyper-coagulability.
Mild disease
Nirmatrelvir/ritonavir (Paxlovid) is a direct acting antiviral medication that inhibits the SARS-CoV-2 3CL protease, recently approved by Health Canada. Data from the EPIC-HR study demonstrated an 89% reduction in the primary endpoint of hospitalization or death among unvaccinated non-hospitalized high-risk adults with microbiologically confirmed infection when treatment was initiated within three days of symptom onset. Pharmacist consultation is strongly recommended to support safe management of drug-drug interactions. The working group recommends nirmatrelvir/ritonavir for use in patients at high risk for progression to severe disease when drug interactions or clinical circumstances provide a favourable risk-benefit balance.
Remdesivir for high-risk outpatients – The PINETREE trial [2] demonstrated an 87% reduced risk of hospitalization in high-risk patients. Most jurisdictions now recommend remdesivir for early treatment of those likely to end up in hospital. Disadvantages of remdesivir include requirement for daily IV administration and cost, while potential benefits include reduction in need for, or duration of, hospital stay. The working group recommends the use of remdesivir as early treatment (within seven days of the onset of symptoms) for patients at very high risk of hospitalization who cannot take alternative oral medications.
Anti-SARS-CoV-2 monoclonal antibodies (moAb) – Randomized controlled trials have demonstrated benefit for specific moAb infusions [3,4,5] in mild disease for patients at high risk of progression. However, monoclonal antibodies are subject to immune evasion with evolving variants. There are currently no approved monoclonal antibodies available for therapy in Canada that are appropriate for the circulating omicron variants.
Moderate to severe disease
Dexamethasone, 6 mg for 10 days, or until hospital discharge, has been demonstrated to reduce mortality in hospitalized patients in large, randomized clinical trials [6]. Dexamethasone is strongly recommended for patients requiring oxygen supplementation as a result of COVID-19. However, a signal for harm in patients with mild disease suggests that steroids be withheld in patients with no or mild hypoxia – especially if explained by another health condition (e.g., heart failure). One study, and some expert opinion, suggests potential benefit for 12 mg [7], although its precise role is not clear. The working group felt that, given this uncertainty, this dose should be limited to the critical care setting, meriting a “neither recommend nor discourage” recommendation until further data are available.
IL-6 inhibitors and targeted therapies – tocilizumab (moAb to the IL-6 receptor) administered within 14 days of hospital admission and within 24 hours of life-support initiation is associated with reduced disease progression and death in patients who are critically ill and require high-flow oxygen, or those who have evidence of systemic inflammation with rapid progression [8,9]. While there is demonstrated benefit for tocilizumab in patients with less severe disease but high CRP or clinical decline despite steroid therapy [10], drug shortages may favour use in more severely ill patients to maximize benefit. When supply concerns are not significant and in the absence of contraindications, the use of targeted immune therapies in addition to steroids is recommended in patients requiring oxygen supplementation due to COVID-19 pneumonia [11]. While tocilizumab is the preferred agent, sarilumab (moAb to IL-6 receptor), tofacitinib (JAK inhibitor) [12], or baricitinib (JAK inhibitor) [13] can be considered alternatives if tocilizumab is not available. Only one of these agents should be administered, based on local availability.
Therapeutic anticoagulation has demonstrated reduced progression to high-flow oxygen for moderately ill patients requiring supplemental oxygen but not organ support [14]. Hospitalized (non-ICU) patients requiring oxygen should be offered therapeutic anticoagulation with low molecular weight heparin (preferred) or unfractionated heparin within 72 hours of admission, to be continued for 14 days or until discharged unless they have a high risk of bleeding. Emerging data suggest that therapeutic anticoagulation should be discontinued if the patient progresses to ICU admission [15]. Initiation of therapeutic anticoagulation should not occur empirically in the ICU in the absence of an alternative indication. Prophylactic dosing anticoagulation is recommended for hospitalized patients if therapeutic dosing is not used.
Remdesivir for moderate-severe disease has been studied in hospitalized populations [16,17] and has demonstrated decrease in the duration of illness, with benefits primarily in patients on low-flow oxygen. Data from Canadian Treatments for COVID‑19 (CATCO) have shown some benefit in terms of reduced progression to ventilation; however, reduction in mortality has been less clear. The use of remdesivir in admitted in-patients on low-flow oxygen is variable across the country. There is less evidence of benefit for people who are already on high-flow oxygen, although some clinicians on a case-by-case basis will use it for patients who are likely unable to clear the virus. The working group recommends the use of remdesivir for patients on low-flow oxygen admitted to hospital; it neither recommends nor discourages its use in patients on high-flow oxygen.
CONTROVERSIES
Budesonide has been studied in two RCTs with variable patient populations [18,19] and appears to reduce time to subjective recovery. However, small sample sizes, open-label design, and low event rates hinder the applicability of the results. While inhaled budesonide is accessible with a reassuring safety profile, its costs and uncertain benefit limit its use. The working group neither recommends nor discourages the use of budesonide in mild disease.
Fluvoxamine is a selective serotonin reuptake inhibitor. As an agonist for the sigma-1 receptor, it may also control inflammation. It has been trialled for mild disease [20,21] and decreases clinical deterioration, hospitalization, and death. It is unclear if results from the Brazilian trial are generalizable; it had a less pertinent outcome (6-hour emergency department visit or admission as a combined endpoint) and a high event rate in the placebo arm, which likely does not reflect the risk for vaccinated patients and populations with lower event rates. Fluvoxamine use is complicated by drug interactions and relatively high dosing compared to its other indications. If used, significant risk of adverse events and drug-drug interactions require pharmacist evaluation to avoid inadvertent harm. The working group neither recommends nor discourages the use of fluvoxamine in mild disease.
RECOMMENDATIONS AGAINST
The working group has identified the following drugs through review of negative trials and clinical experience. These are drugs that should not be given in any patient population, except in active clinical trials.
Hydroxychloroquine is an antimalarial that was initially thought to have significant promise based on in vitro data [23] and some observational studies [24,25]. However, large, international randomized trials failed to show benefit [26,27] and had potential signals for harm [28].
Ivermectin is possibly the most contentious medication proposed in the treatment of COVID-19. While anecdotal and observational trials initially signalled a possible benefit [29], critical appraisal of the data determined methodological flaws, leading to retractions of published articles. Randomized trials have not demonstrated benefit [30]. The widespread use of ivermectin for COVID-19 is exacerbating shortages for patients with vermicidal indications, while use of veterinary formulations has resulted in toxicity in others [31,32]. Medical colleges in Canada actively recommend against the use of ivermectin for treatment of COVID-19 with the potential for disciplinary action for non-compliance [33,34].
Azithromycin was initially included as part of combination therapy in case series from France [35]; however, further studies have shown little benefit [36,37] unless it is being used to treat an identified bacterial infection (see below).
Antibiotic therapy, while potentially lifesaving in the presence of a bacterial infection, should not be routinely used for patients admitted with COVID-19 since bacterial co-infection is rare, between 2% and 8% [38,39]. Bacterial pneumonia can develop during hospitalization, and antibiotics may need to be considered for severe and critical disease if a co-infection is suspected (e.g., acute worsening after a period of improvement/stability or new focal consolidation). The working group was divided on the empirical use of anti-bacterials for patients with severe and critical disease. While antibiotics may treat bacterial super-infections, they occur in a minority of patients. Regardless, the working group agreed that if antibiotics are given initially, a strategy for rapid de-escalation is critical.
Colchicine has been studied in mild disease and showed non-significant benefit in patients over 40 years of age with at least one risk factor for disease progression [22]. However, this therapy is limited by a number needed to treat (NNT) of 71, pertinent side effects, and contraindications. Its role in vaccinated patients is unclear, although it continues to be studied in clinical trials. The working group does not recommend colchicine for mild illness.
Other therapies that have inconsistent evidence of benefit or evidence of harm include convalescent plasma, interferon, and lopinavir/ritonavir. While bamlanivumab, casirivimab/imdevimab, and sotrovimab may have been beneficial against the original SARS-CoV-2 and select subsequent variants, the current dominant strains (omicron at the time of writing) render them ineffective. There is little evidence to support the regular use of NSAIDs or routinely altering existing therapy with angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs). Supplementation with vitamin C, D,
or E have not shown benefit.
CONCLUSION
This AMMI Canada Practice Point provides a concise framework to guide the clinical care of adults with COVID-19. With constantly evolving information, the working group will continue to evaluate and incorporate data that inform clinical practice, particularly in the context of new variants, vaccine efficacy, and the availability of novel therapeutics. The working group will update this document periodically.
REFERENCES
1. Levin MJ, Ustianowski A, De Wit S, et al. Intramuscular AZD7442 (tixagevimab–cilgavimab) for prevention of Covid-19. N Engl J Med. 2022;386:2188–200. https://doi.org/10.1056/NEJMoa2116620. Medline:35443106
2. Gottlieb RL, Vaca CE, Paredes R, et al. Early remdesivir to prevent progression to severe Covid-19 in outpatients. N Engl J Med. 2022;386:305–15. https://doi. org/10.1056/NEJMoa2116846. Medline:34937145
3. Weinrech DM, Sivapalasigam S, Norton T. REGEN-COV antibody combination and outcomes in outpatients with Covid-19. N Engl J Med. 2021;385:e81.
4. Recovery collaborative group. https://www.medrxiv. org/content/10.1101/2021.06.15.21258542v1.full.pdf (Accessed Dec. 23, 2021)
5. Gupta A, Gonzalez-Rojas Y, Juarez E, et al. Early treatment for COVID-19 with SARS-CoV-2 neutralizing antibody sotrovimab. N Engl J Med. 2021;385:1941– 50. https://doi.org/10.1056/NEJMoa2107934. Medline:34706189
6. RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. https://doi.org/10.1056/NEJMoa2021436. Medline:32678530
7. The COVID STEROID 2 Trial group. Effect of 12 mg vs 6 mg of dexamethasone on the number of days alive without life support in adults with COVID-19 and severe hypoxemia, the COVID STEROID 2 randomized trial. JAMA. 2021;326(18):1807–17.
8. The REMAP-CAP Investigators. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med. 2021;384:1491–1502. https://doi. org/10.1056/NEJMoa2100433. Medline:33631065
9. RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397(10285):1637–45.
10. RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397(10285):1637–45.
11. Agarwal A, Rochwerg B, Lamontagne F, et al. A living WHO guideline on drugs for Covid-19. BMJ. 2020;370:m3379. https://doi.org/10.1136/bmj.m3379. Medline:32887691
12. Guimaraes PO, Quirk D, Furtado RH. Tofacitinib in patients hospitalized with COVID-19 pneumonia. N Engl J Med. 2021;385(5):406–15.
13. Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2021;384:795–807.
14. Goligher EC, Bradbury CA, McVerry BJ, et al. Therapeutic anticoagulation with heparin in critically ill patients with Covid-19. N Engl J Med. 2021;385:777– 89. https://doi.org/10.1056/NEJMoa2103417. Medline:34351722
15. REMAP-CAP. Domain-specific appendix COVID-19 anti-coagulation. https://static1.squarespace.com/ static/5cde3c7d9a69340001d79ffe/t/60457a757023b06 241b1453c/1615166074587/REMAP-CAP+-+ Therapeutic+Anticoagulation+-+V3+-+ 27+February+2021_WM.pdf (Accessed Jan. 26, 2021)
16. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19 – final report. N Engl J Med. 2020;383:1813–26. https://doi.org/10.1056/ NEJMc2022236
17. WHO Solidarity Trial Consortium. Repurposed antiviral drugs for Covid-19 – Interim WHO solidarity trial results. N Engl J Med. 2021;384:497–511. https://doi.org/10.1056/NEJMoa2023184. Medline: 33264556
18. Rmakrishnan S, Nicolau DV, Langford B, et al. Inhaled budesonide in the treatment of early COVID-19 (STOIC): a phase 2, open-label, randomised controlled trial. Lancet Respir Med. 2021;9(7):763–72. https://doi.org/10.1016/S2213-2600(21)00160-0
19. Yu LM, Bafadhel M, Dorward J, et al. Inhaled budesonide for COVID-19 in people at high risk of complications in the community in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial. Lancet. 2021;398(10303):843–55. https://doi.org/10.1016/ S0140-6736(21)01744-X
20. Lenze EJ, Mattar C, Zorumski, et al. Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial. JAMA. 2020;324(22):2292–300.
21. Reis G, Moreira-Silva E, Silva D, et al. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. Lancet Glob Health. 2021;S2214-109X(21):00448-4. https://doi.org/10.1016/S2213-2600(21)00222-8
22. Tardif JC, Bouabdallaoui N, L’Allier PL, et al. Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Resp Med. 2021;9(8):924–32.
23. Liu J, Cao R, Xu M, et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. https://doi.org/10.1038/s41421-020-0156-0. Medline:32194981
24. Million M, Gautret P, Colson P, et al. Clinical efficacy of chloroquine derivatives in COVID-19 infection: comparative meta-analysis between the big data and the real world. NMNI. 2020;38:100709. https://doi. org/10.1016/j.nmni.2020.100709. Medline:33088574
25. Gautret P, Lagier JC, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of OVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56(1):105949. https://doi.org/10.1016/j.ijantimicag.2020.106243. Medline:33408014
26. WHO solidarity trial consortium. Repurposed antiviral drugs for Covid-19 – interim WHO solidarity trial results. N Engl J Med. 2021;384:497–511. https://doi. org/10.1056/NEJMoa2023184. Medline:33264556
27. The recovery collaborative group. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020;383:2030–40. https://doi. org/10.1056/NEJMoa2022926. Medline:33031652
28. Ghazy RM, Almaghraby A, Shaaban, et al. A systematic review and meta-analysis on chloroquine and hydroxychloroquine as monotherapy or combined with azithromycin in COVID-19 treatment. Nature Sci Rep. 2020;10:22139. https://doi.org/10.1038/s41598- 020-77748-x. Medline:33335141
29. Popp M, Stegemann M, Metzendor M, et al. Ivermectin for preventing and treating COVID-19. Cochrane Database Syst Rev. 2021;28;7(7):CD015017. https://doi.org/10.1002/14651858.CD015017.pub2. Medline:34318930
30. Roman YM, Burela PA, Pasupuleti V, et al. Ivermectin for the treatment of coronavirus disease 2019: a systematic review and meta-analysis of randomized controlled trials. Clin Infect Dis. 2022;74:1022–9. https:// doi.org/10.1101/2021.05.21.21257595
31. Leung E, Raybardhan S, Graham C, et al. Ivermectin treatment for strongyloides infection in patients with COVID-19. Can Commun Dis Rep. 2021;47(7/8):316–21. https://doi.org/10.47326/ ocsat.2021.02.30.1.0
32. Temple C, Hoang R, Hendrickson RG. Toxic effects from ivermectin use associated with prevention and treatment of Covid-19. N Engl J Med. 2021; 385:2197– 219. https://doi.org/10.1056/NEJMc2114907. Medline:34670041
33. BC College of Physicians. Joint message about ivermectin in the prevention and treatment of COVID-19. https://www.cpsbc.ca/files/pdf/2021-10-01-Joint- Message-about-Ivermectin-in-the-Prevention-and-Treatment-of-COVID-19.pdf (Accessed Jan. 26, 2022).
34. Alberta College of Physicians https://cpsa.ca/news/joint-statement-from-cpsa-and-acp-regarding-inappropriate-prescribing-and-dispensing-of-ivermectin-to-treat-or-prevent-covid-19/(Accessed Jan 26, 2022).
35. Guerin V, Levy P, Thomas JL, et al. Azithromycin and hydroxychloroquine accelerates recovery of outpatients with mild/moderate COVID-19. AJMAH. 2020:45–55. https://doi.org/10.9734/ajmah/2020/ v18i730224
36. Cavalcanti A, Zampieri F, Rosa R, et al. Hydroxychloroquine with or without azithromycin in mild-to-moderate Covid‑19. N Engl J Med. 2020;383:2041–52. https://doi.org/10.1056/ NEJMx200021. Medline:33210858
37. Hinks TS, Cureton L, Knight R, et al. Azithromycin versus standard care in patients with mid-to-moderate COVID-19 (ATOMIC2): an open-label, randomised trial. Lancet Respir Med. 2021;9(10):1130–40. https://doi.org/10.1016/S2213-2600(21)00263-0
38. Russell CD, Fairfield CJ, Drake TM et al. Co-infections, secondary infections, and antimicrobial use in patients hospitalised with COVID-19 during the first pandemic wave from the ISARIC WHO CCP-UK study: a multicentre, prospective cohort study. Lancet Microbe. 2021;2:e354–65. https://doi.org/10.1016/ S2666-5247(21)00090-2
39. Langford BJ, So M, Raybardhan S et al., Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis, Clinical microbiology and infection. Clin Microbiol Infect. 2021;27:520e531. https:// doi.org/10.1016/j.cmi.2020.12.018. Medline:33418017


