Joanne Andrew, BA, RN, MSc, CIC1* and Debbi Marais, PhD2
1 Infection Prevention and Control, Island Health, BC, Canada
2 University of Warwick, Gibbet Hill, Coventry, United Kingdom
*Corresponding author:
Joanne Andrew
Island Health, BC, Canada
email: This email address is being protected from spambots. You need JavaScript enabled to view it.
ABSTRACT
Background: Healthcare-associated infections (HAI) present a significant risk to patients globally and they are listed as one of the most frequent adverse events in healthcare. The use of personal protective equipment (PPE) is one method of reducing transmission, yet despite the benefits of appropriate PPE being well documented, compliance by healthcare workers is poor. The aim of this study was to assess nurses’ ideas to improve compliance with PPE when caring for patients on additional precautions.
Methods: The study took place at a 148-bed acute care hospital in British Columbia, Canada. A total of eight nurses, both licensed practical nurses (LPNs), and registered nurses (RNs) were selected from across the different wards based on their ability to provide the information required for the research study. Data was collected using qualitative semi-structured interviews to the point of data saturation, and consensus was obtained following the Delphi technique.
Results: Eight themes emerged from the coding: risk assessment, knowledge/education, time/staffing, visible leadership, COVID-19 pandemic, patients, ward culture and PPE audits. The results were separated into two groups, influences on compliance and ideas for improving compliance.
Conclusion: All eight themes contributed to the perception of risk which was identified as having the greatest influence on PPE compliance. These findings highlight the need for further research into the multifactorial approach to improving PPE compliance drawing from healthcare workers perspective.
KEYWORDS
PPE, compliance improvement, nurses, acute care
INTRODUCTION
Healthcare-associated infections (HAI) present a significant risk to patients globally, they are an important patient safety and quality issue due to the associated increased morbidity and mortality, and they are listed as one of the most frequent adverse events in healthcare. (Public Health Agency of Canada, 2022; World Health Organisation, 2022). The first global report on infection prevention and control (IPAC) released by the World Health Organisation (WHO) in May 2022 estimates that for every 100 patients admitted to the hospital in high-income countries, at least seven will acquire at least one HAI and this number is double for low- to middle-income countries (WHO, 2022). In 2013, the Public Health Agency of Canada (PHAC) reported more than 200,000 HAIs, resulting in more than 8,000 deaths in Canadian hospitals (Public Health Agency of Canada, 2013) and in 2017, it was estimated through a point prevalence study of participating hospitals in Canada, that 7.9% of in-patients had at least one HAI (Public Health Agency of Canada, 2020).
Surveillance for HAIs in Canada is managed by PHAC through the Canadian Nosocomial Infection Surveillance Program (CNISP). CNISP, a collaboration between PHAC, the Association of Medical Microbiology and Infectious Disease Canada, and participating Canadian Hospitals was established in 1994 with just 18 participating Canadian hospitals at the time (Public Health Agency of Canada, 2022). Although the number of participating hospitals has increased over the years to 90, this is a far cry from the 1,300 hospitals across Canada (Blair, 2023). Therefore, the true burden of HAIs in Canada could be significantly underrepresented.
HAIs are estimated to have cost Canadian healthcare $281 million from 2014-2015 (Canadian Patient Safety Institute, 2016). Yet, it is estimated that 55-70% of healthcare-associated infections can be prevented by increasing and improving a range of IPAC interventions (Bearman et al., 2021; WHO, 2022). While hand hygiene has been suggested as the most effective intervention for reducing HAI (IPAC Canada, N.D; Public Health Agency of Canada, 2021),other prevention methods should not be underestimated.
The use of personal protective equipment (PPE) is identified in both routine practice (RP) and additional precautions (AP) as a method of reducing the risk of transmission of potentially infectious microorganisms to healthcare workers (McCarthy et al., 2020; Reddy et al., 2019). When used appropriately, PPE can interrupt the mode of transmission by protecting the wearer and breaking the chain of infection. Despite the benefits of appropriate PPE use being well documented (Williams et al., 2019), low compliance with PPE use by healthcare workers remains a worldwide concern (Smith et al., 2021; Van Gulik et al., 2021; Haile et al., 2017). The aim of this study was to assess nurses’ ideas to improve compliance with PPE when caring for patients on additional precautions.
METHODS
Research method
The study was conducted in a 148-bed community hospital on Vancouver Island, British Columbia, Canada to explore ideas from nurses who are working directly with patients on additional precautions, on how to improve PPE compliance. The Delphi Technique was used as qualitative research method of choice. This method was chosen due to its foundation in obtaining information and learning from highly experienced practitioners. Additionally, the Delphi technique supports a research process that not only identifies each of the contributing solutions, but helps to identify priority or importance.
Ethical approval
Before commencing the research project, ethical approval was sought through both University of Essex and the Health Authority Research Ethics Board (HREB). Participation in the study was voluntary, participants were provided with information regarding the study, including confidentiality and data management. Consent was sought and received from all participants, and no incentives were provided.
Sampling approach
Non-probability sampling methods were reviewed, and purposive sampling was selected as the sampling method as it is based on a phenomenon of interest. Participants were chosen based on their knowledge or experience in addition to their willingness to participate (Creswell & Plano Clark, 2011). Nurses, both LPNs, and RNs were selected from across the different wards based on their ability to provide the information required for the research study. A total of eight nursing staff were interviewed from across the different wards within the hospital. Interviews lasted between 30 to 45 minutes. Although some studies suggest a larger number of participants are required to achieve data saturation (Guest et al., 2006), there are other studies which argue that data saturation can in fact be achieved even with small sample sizes particularly with homogenous study populations (Hennick & Kaiser, 2022).
Recruitment
The intention of recruitment for this research study was to obtain representation from across the nursing profession and in-patient wards. The recruitment strategy included attending team meetings and report handover on the in-patient wards, and placing and emailing posters advertising the research opportunity. Interested applicants were requested to contact the researcher in person, by email, or by telephone expressing their interest.
All participants were screened to confirm inclusion and exclusion criteria. Inclusion criteria included the designations of nurses who provide care to patients on additional precautions in an acute care setting. Exclusion criteria included nurses who were not currently in an active role, e.g., on maternity leave, and those who had not been working in the role for at least the last six months.
Data collection and analysis
A focus group study was initially considered as an appropriate method of data collection for this particular research study. However, consideration was given to low staffing levels at the hospital during the pandemic, and the inability of leadership to release a number of staff at the same time to attend focus group sessions. After discussion with ward managers, interviews were chosen as a suitable alternative. The interviews were conducted face-to-face, following a semi-structured approach, and were recorded. Each participant was asked to provide their thoughts and opinions on the influences of education, ward culture, leadership, ergonomics, and patient involvement on staff compliance with PPE use. These factors were identified in the literature search as having a potential influence on PPE use. Participants were subsequently encouraged to share additional thoughts, ideas, and strategies to improve PPE compliance. Interviews were completed to the point of data saturation. Reflexive Thematic Analysis was used to code and theme the data (Braun & Clarkes, 2006).
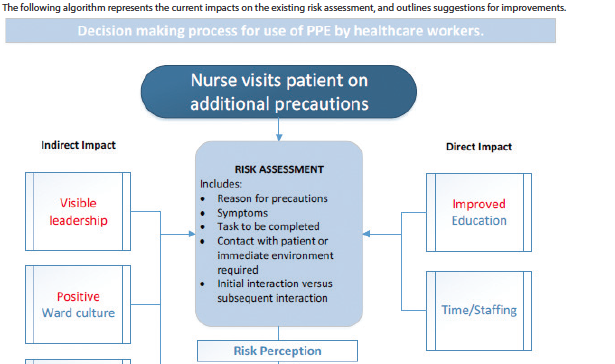
Two rounds of coding were completed, and the following eight themes were identified as shown in Figure 1. Once the themes were identified, a series of statements were created and emailed to the participants to obtain feedback and consensus. The statements consisted of the following:
1. Risk assessment forms the basis of my decision to wear or not to wear PPE when providing care to a patient on additional precautions. Four main factors contribute to
my point-of-care risk assessment these include: Task to be completed (contact or no contact with the patient), level of fear of transmission (to myself, my family and my patients), knowledge of my patient (symptoms, compliance), and time (staffing levels/workload).
2. Education is the most important influence on PPE use as it provides the knowledge that underpins good risk assessment. It can be difficult to receive education but the best way to provide it is in short one-on-one sessions, in-the-moment opportunities, or by email.
3. The infection control practitioner (ICP), Clinical Nurse Leader (CNL), and Clinical Nurse Educator (CNE) should all support infection prevention and control education and information by being able to answer questions, support staff decision-making, and support good practice.
4. Regular PPE audits are a good way to help improve compliance, they serve as a reminder for good practice, and I would want my unit to do well.
5. Providing competent patients with education about additional precautions, including the requirements for themselves and staff, would have a positive impact on staff PPE use.
RESULTS AND DISCUSSION
Five of the eight participants responded and other than minor changes, there was consensus on all the statements. No further follow up was required.
BARRIERS AND FACILITATORS TO COMPLIANCE
Barriers to healthcare worker compliance with PPE use have been well studied and include issues such as ill-fitting or lack of access to PPE, poor understanding of current policies relating to PPE use, risk perception, high workload, and workplace culture (Brooks et al., 2021; Houghton et al., 2020).
While there are many studies identifying barriers to compliance, there are limited studies that focus on healthcare workers' perspective on ways to improve compliance with PPE use (Efata et al., 2021). Additionally, other articles focus mainly on improving adherence to RP, of which PPE is only a part, and the more recent articles refer to PPE use specifically concerning the COVID-19 pandemic where it could be assumed that PPE compliance is improved (Beckman et al., 2013; Tawfiq &
Auwaerter, 2019).
1. Exploring current influences on ppe compliance
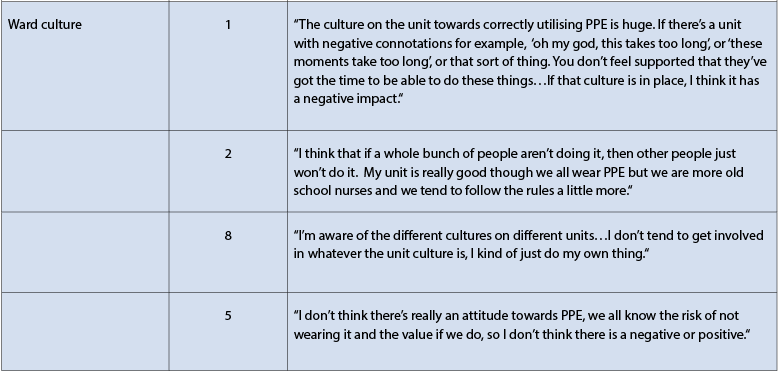
Table 1 provides a sample of quotes from participants to illustrate how the themes address the objective to explore the thoughts and opinions of nurses on the influences that impact compliance with PPE use.
1.1. Risk perception
The most significant influence on PPE compliance is unequivocally nurses’ perception of risk, with fear of transmission being the main driver for PPE use, this is reflective of findings from both Haile et al. (2017) and Harrod et al. (2020). When performing their own risk assessment, the mode of transmission associated with the type of additional precautions influenced compliance and it was noted that staff were more likely to wear the appropriate PPE when a patient was on droplet and contact precautions as opposed to just contact precautions. Staff do not only assess the transmission method; they also assess the type of interaction that is to take place within the patient space. Participants identified that they would more likely use appropriate PPE when interacting directly with the patient, as opposed to just the patient environment (Table 1).
1.2. Risk assessment
Participants identified that when working with patients on additional precautions, they modify their PPE use under certain conditions. Although there is a standardized risk assessment tool based on Canada-wide guidance (IPAC Canada, 2022), staff adapt this risk assessment to include additional factors based on their knowledge of the disease, the patient’s current symptoms, and type of contact required with the patient and their environment. Furthermore, in addition to modifying the risk assessment tool, other factors contributed significantly to the staff’s ability to perform an informed and accurate risk assessment. These included education, culture, and time/staffing. It was evident from the interviews, that participants do not always have sufficient or accurate knowledge to make fully informed risk assessments, as such may be unintentionally putting themselves and their patients at increased risk of transmission.
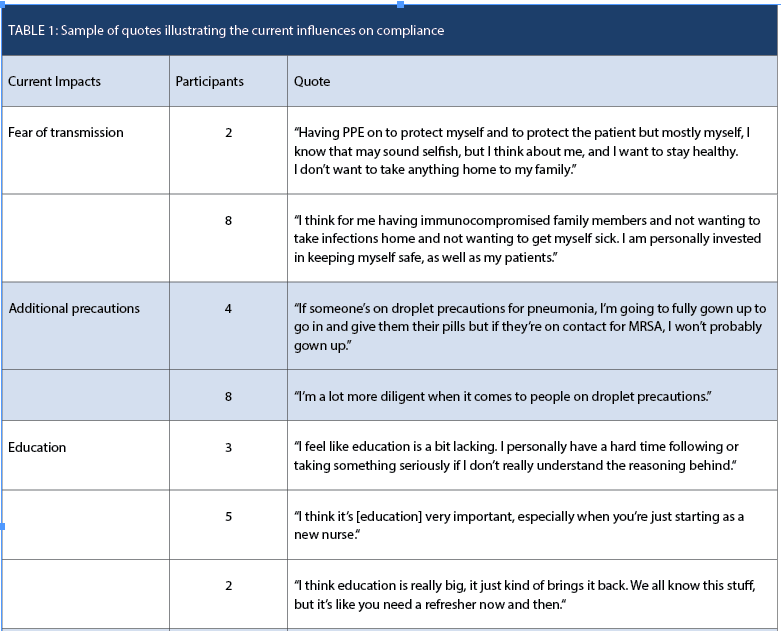
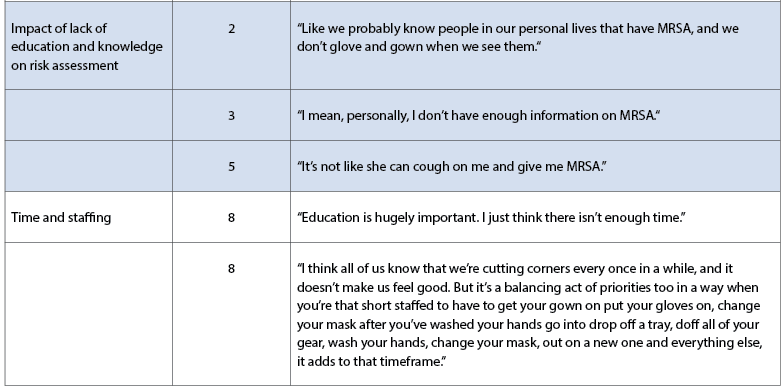
1.2.1. Direct influences on risk assessment – time and staffing
Participants acknowledged that IPAC education was important, but also recognised that receiving education was significantly hindered by lack of time which is directly related to low staffing levels and high hospital census rates. Participants identified that constant improvements in technology, equipment, and computerised systems meant that the need for education was continuous despite the lack of dedicated time, leadership support, and lack of relief cover to complete it. These findings are consistent with other studies such as Lalonde et al. (2013) Shadadi et al. (2018) and Coventry et al. (2015).
1.2.2. Indirect influence on risk assessment – culture and environment
Ward culture, defined for the purpose of this study as the overall attitude of nurses and leadership on the ward towards the importance of compliance with PPE, was not identified as having a significant impact on nurses’ choice to use PPE. Participants recognised that while culture can influence choice, there are additional factors such as risk assessment which have a greater influence on their decision to use or not to use PPE (Table 1). Additionally, participants were asked about environmental impact, such as ergonomics, and how that may influence PPE compliance. Participants did not identify environmental design as having a noteworthy impact on PPE compliance.
1.3. COVID-19 pandemic
The COVID-19 pandemic raised awareness of the importance of PPE in protecting staff and their patients against transmission. Staff intimated that the increased and dedicated education they received during the pandemic had raised awareness of the importance of PPE use, and influenced an improvement in compliance. However, it was pointed out during the interviews that recent site audits have identified a reduction in PPE compliance despite still being in a pandemic. Overall, despite the additional education and raised awareness of the importance of PPE use, staff still rely on their own risk assessment to direct their PPE use. Staff are now significantly less concerned about COVID-19 than they were at the beginning of the pandemic. This has resulted in a lower risk perception and subsequent reduction in PPE compliance. With that being said, there are still positive and possibly permanent changes associated with the pandemic, however, it is unclear if the improvement in practice is based on just one factor, such as increased risk, or multiple factors combined, including risk, knowledge increase, improved education and culture change (Table 1).
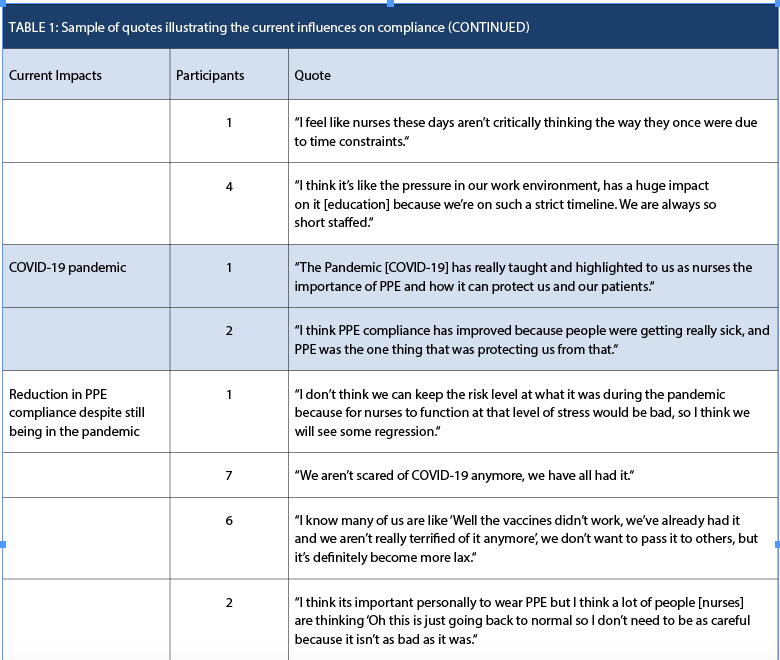
2. Exploring ways to improve compliance
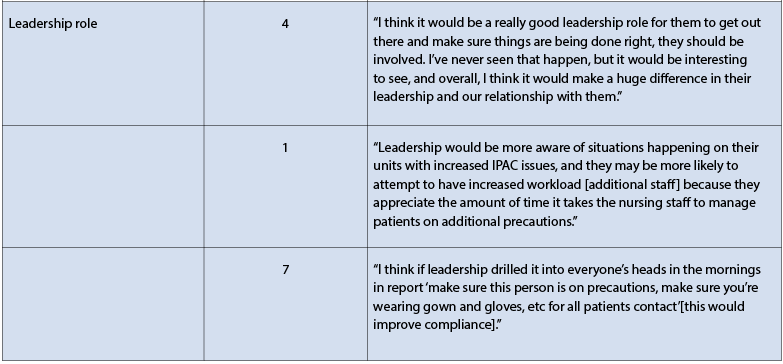
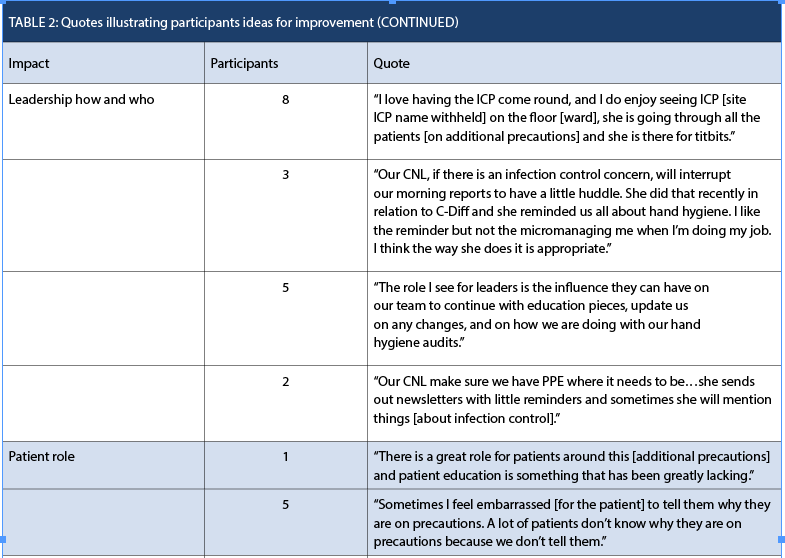
Table 2 provides a sample of quotes from participants to illustrate how the themes address ideas to improve compliance.
2.1. Education
Education was identified as a key contributor to compliance as IPAC knowledge informs how staff perform their risk assessments. However, it was also recognised that staffing levels and hospital census significantly impact staff’s ability to access education when offered using traditional methods such as classroom sessions. Participants identified that due to operational limitations, examples of the best ways to receive education include short sessions held directly on the unit, one-on-one or in-the-moment quick sessions, email education, or newsletters. Staff also felt that education that focused on disease and transmission would support an informed risk assessment (Table 2).
2.2. Patients
There is a plethora of information that identifies that partnering with patients improves health outcomes and patient satisfaction (Krist et al., 2017). In the current study, some participants identified that staff will sometimes avoid having conversations about additional precautions with patients due to their lack of knowledge or confidence in doing so. The concept of patient education regarding additional precautions, including the expectation of PPE use by staff, was presented to participants as a conceivable way to increase compliance based on studies by Alzyood et al. (2018) and Butenko et al. (2017). Intriguingly, participants were generally positive about the inclusion of patients and felt that it would most likely improve healthcare workers compliance with PPE use. Interestingly, none had particularly thought about involving patients in this way previously, or the impact this may have on staff PPE compliance (Table 2).
2.3. Leadership
Participants discussed that they find the support of their clinical nurse leaders helpful and identified that increased knowledge of IPAC practices, and reminders to staff about best practice undoubtedly have a positive impact on compliance. However, they also sympathized with their CNLs and recognized how busy they were already, running the unit and managing day-to-day issues. ICPs were highlighted as a strong resource for improving compliance, however, it was also acknowledged that their in-person time on the unit is limited and as such, their ability to provide comprehensive support was restricted. On the other hand, senior site leadership such as managers and the site director were not currently associated with having any impact on PPE compliance. In addition to improving PPE compliance directly, there was also discussion about the impact leadership roles have on ward culture and the subsequent potential for indirect positive influence on PPE compliance. Positive role modelling and organizational culture have been identified in multiple studies as having a positive influence on IPAC practices. (Gilbert et al., 2019; Barratt et al., 2020; Peponis et al., 2017). Haile et al. (2017) noted that compliance with IPAC practices was improved by up to 2.23 times when healthcare staff had strong management support for safe environments and infection prevention and control (Table 2).
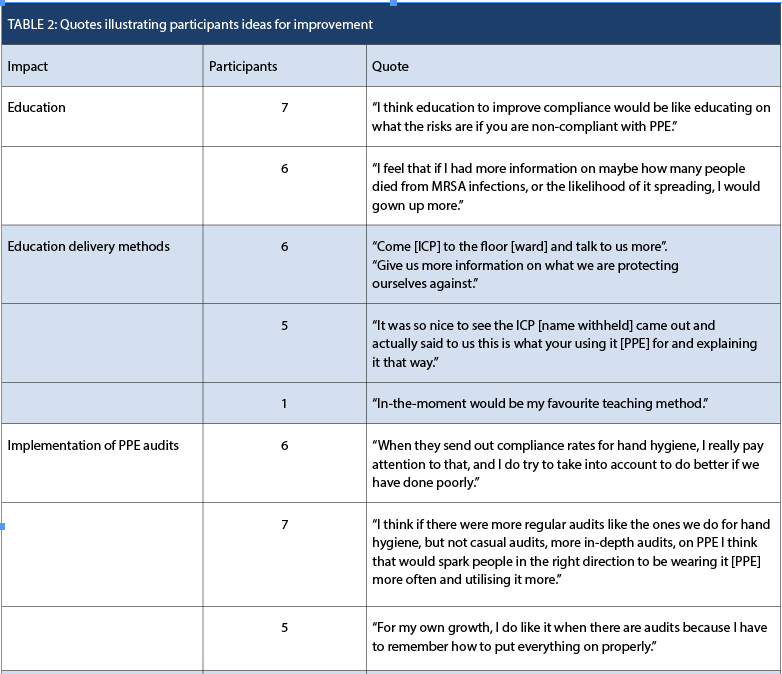
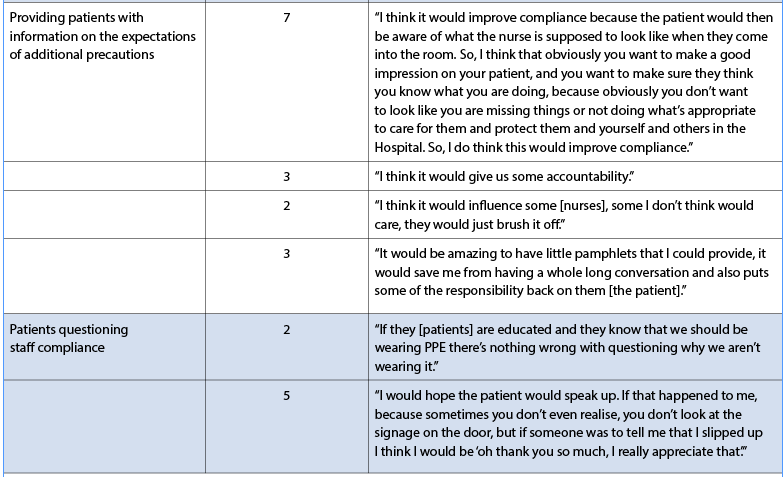
2.4. Audits
IPAC programs have continuously focused on implementing interventions designed to improve compliance such as education and audits (Hon et al., 2008; Larson et al., 2013). Participants identified that they found the current hand hygiene audits helpful and identified that they have a positive effect on compliance as they act as a continuous reminder of good practice. It was, therefore, felt that introducing PPE audits on the units would provide additional opportunities for in the moment teaching (Table 2).
LIMITATIONS
This study was carried out at only one acute care hospital out of 11 within the health authority. Although the hospitals differ in size, the challenges around staffing, time, and census are similar across the region. There are some differences in the physical environment due to newer buildings offering private patient rooms and more space. However, participants did not identify environment as having an impact on PPE compliance.
Staffing issues at the site presented significant difficulties in enrolling participants in the research study. Many staff were interested and keen to take part but opted out based on their increased workload and the inability of colleagues to cover them while they attended the interview.
As a result, only eight participants were interviewed. Despite the small sample size, it was evident early in the interviews that information saturation would be reached even with a lower number of participants. Additionally, during the follow-up, as part of the Delphi process, a consensus was reached with the first round of follow-up questions and although there were only five respondents, comments were based on minor word changes only, and as such, it can be assumed that there would have been no significant changes had more participants responded.
CONCLUSION AND RECOMMENDATIONS
There is no doubt that the appropriate use of PPE serves to protect both patients and staff from the transmission of infectious pathogens. Improving staff compliance with PPE use is an ongoing challenge for which there appears to be no single answer or intervention. Rather, a combination of factors contributes to risk assessment and decision-making. Staff use their own risk assessment in conjunction with existing approved risk assessments and recommendations, to decide how and when to use PPE. However, their personal risk assessment may be flawed due to it being based on incomplete or inaccurate information, and staff may be inadvertently putting themselves or their patients at increased risk of transmission.
This study provides key considerations for improving compliance, a package or bundle of quality improvements is recommended:
• Improved education opportunities supported by innovative ways to deliver short education sessions designed to meet the time and staffing challenges of today’s nurses.
• Education that focuses on disease and modes of transmission in addition to point of care risk assessment and PPE use so that nurses have the right information when assessing risk.
• Promotion of visible leadership provided by a multidisciplinary leadership team aimed at championing IPAC best practices through role modelling and promoting positive culture change.
• Engaging patients as partners when they are on additional precautions by providing them with educational material designed to promote health literacy and improve staff compliance.
• Implementation of regular PPE audits to support change. Audits should include in-the-moment feedback and opportunities for teaching, results should be shared and supported by incentives where possible.
It is recognised that while this is a small study, the results highlight the need for further research to better understand the complexity of a multi-interventional approach to improving nurses compliance to PPE use when caring for patients on additional precautions.
REFERENCES
1. Alzyood, M., Jackson, D., Brooke, J. & Aveyard, H. (2018). An integrative review exploring the perceptions of patients and healthcare professionals towards patient involvement in promoting hand hygiene compliance in the hospital setting. Journal of Clinical Nursing. 27:1329–1345. DOI: 10.1111/jocn.14305.
2. Barratt, R., Gilbert, G. Shaban, R. Wyer, M. & Hor, S. (2020). Enablers of, and barriers to, optimal glove and mask use for routine care in the emergency department: an ethnographic study of Australian clinicians. Australian Emergency Care 23(2):105-113. DOI: 10.1016/j.auec.2019.10.002.
3. Bearman, G., Doll, M., Cooper, K. & Stevens, M. (2019) Hospital Infection Prevention: How Much Can We Prevent and How Hard Should We Try? Current Infectious Disease Reports 21:2. DOI: https://doi.org/10.1007/s11908-019-0660-2.
4. Beckman, S. et al. (2013) Evaluation of respiratory protection programs and practices in California hospitals during the 2009-2010 H1N1 influenza pandemic. American Journal of Infection Control 41(11):1024-1031. DOI: 10.1016/j.ajic.2013.05.006.
5. Blair, N. (2023). Healthcare system statistics in Canada. Available from: https://madeinca.ca/health-care-system-statistics-canada/#:~:text=spending%20in%202017.-,Hospitals%20in%20Canada,and%20on%20Prince%20Edward%20Island.
6. Braun, V. & Clarke, V. (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 77-101. DOI: 10.1191/1478088706qp063oa.
7. Brooks, S., Greenberg, N., Wessely, S. & Rubin, G. (2021). Factors affecting healthcare workers’ compliance with social and behavioural infection control measures during emerging infectious disease outbreaks: rapid evidence review. BMJ Open 11:e049857. DOI: 10.1136/bmjopen-2021-049857.
8. Butenko, S., Lockwood, C. & McArthur, A. (2017). Patient experiences of partnering with healthcare professionals for hand hygiene compliance: a systematic review. JBI Database of Systematic Reviews and Implementation Reports 15:1645–70. DOI: 10.11124/JBISRIR-2016-003001
9. Canadian Patient safety Institute. (2016). Measuring Patient Harm in Canadian Hospitals. Available from: https://secure.cihi.ca/free_products/cihi_cpsi_hospital_harm_en.pdf.
10. Coventry, T., Maslin-Prothero, S. & Smith, G. (2015). Organizational impact of nurse supply and workload on nurses continuing professional development opportunities: an integrative review. Journal of Advanced Nursing 71(12):2715-2727. DOI: https://doi.org/10.1111/jan.12724.
11. Cresswell, J.W. & Plano Clark, V. L. (2011). Designing and conducting mixed method research. 2nd ed. Thousand Oaks: Sage Publishing.
12. Etafa, W., Gadisa, G., Jabessa, S. & Takele, T. (2021). Healthcare workers’ compliance and its potential determinants to prevent COVID-19 in public hospitals in Western Ethiopia. BMC Infectious Disease 21(454). DOI: https://doi.org/10.1186/s12879-021-06149-w.
13. Gilbert, G.L. & Kerridge, I. (2019). The politics and ethics of hospital infection prevention and control: a qualitative case study of senior clinicians’ perceptions of professional and cultural factors that influence doctors’ attitudes and practices in a large Australian hospital. BMC Health Services Research 19:212. DOI: https://doi.org/10.1186/s12913-019-4044-y.
14. Guest, G., Bunce, A., & Johnson, L. (2006). How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods, 18(1), 59-82. DOI: https://doi.org/10.1177/1525822X05279903.
15. Haile, T., Engeda, H. & Abdo, A. (2017). Compliance with Standard Precautions and Associated Factors among Healthcare Workers in Gondar University Comprehensive Specialized Hospital, Northwest Ethiopia. Journal of Environmental and Public Health 2017:2050635. DOI: https://doi.org/10.1155/2017/2050635.
16. Hennik, M. & Kaiser, B. (2022). Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Social Science & Medicine 292:114523 DOI: https://doi.org/10.1016/j.socscimed.2021.114523.
17. Hon, C. et al. (2008). Personal protective equipment in health care: Can online infection control courses transfer knowledge and improve proper selection and use? American Journal of Infection Control 36(10):e33-e37. DOI: https://doi.org/10.1016/j.ajic.2008.07.007.
18. Harrod, M. et al. (2020). A qualitative study of factors affecting personal protective equipment use among health care personnel. American Journal of Infection Control 48(4):410-415. DOI: https://doi.org/10.1016/j.ajic.2019.08.031.
19. Houghton, C. et al. (2020). Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database of Systematic Reviews 4(4):CD13582. DOI: 10.1002/14651858.CD013582.
20. IPAC Canada. (N.D). Information about Hand Hygiene. Available from: https://ipac-canada.org/hand-hygiene.
21. IPAC Canada. (2022) Infection Prevention and Control Core Competencies for Healthcare Providers. Available from: https://ipac-canada.org/photos/custom/pdf/IPAC_CoreCompetencies_2022_web.pdf.
22. Krist, A.H., Tong, S.T. Aycock, R. & Longo, D. (2017). Engaging patients in decision-making and behavior change to promote prevention. Studies in Health Technology and Information 240:284-302. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6996004/.
23. Lalonde, M., McGillis, L., Hall, L., Price, S., Andrews, G., Harris, A. & MacDonald-Rencz, S. (2013) Support and Access for Nursing Continuing Education in Canadian Work Environments. Nursing Leadership 26 (special issue) 51-60. DOI: 10.12927/cjnl.2013.23250.
24. Larson, E. et al. (2013) Impact of Electronic Surveillance on Isolation Practices. Infection Control & Hospital Epidemiology 34(7): 694-699. DOI: 10.1086/671001.
25. McCarthy, R., Gino, B., d’Entremont, P., Barari, A. & Renouf, T. (2020). The Importance of Personal Protective Equipment Design and Donning and Doffing Technique in Mitigating Infectious Disease Spread: A Technical Report. Cureus 12(12): e12084. DOI: 10.7759/cureus.12084.
26. Peponis, T., Cropano, M.C. & Larentzakis, A. (2017) Trauma team utilization of universal precautions: if you see something, say something. European Journal of Trauma and Emergency Surgery 43(1):145–150. DOI: 10.1007/s00068-016-0663-8.
27. Public Health Agency of Canada. (2013). The Chief Public Health Officer’s Report on the State of Public Health in Canada 2013 – Healthcare-associated infections – Due diligence. Available from: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/chief-public-health-officer-report-on-state-public-health-canada-2013-infectious-disease-never-ending-threat/healthcare-associated-infections-due-diligence.html.
28. Public Health Agency of Canada. (2020) Healthcare-associated infections and antimicrobial resistance in Canadian acute care hospitals, 2014–2018. Canada Communicable Disease Report 45(5). Available from: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2020-46/issue-5-may-7-2020/amr-canadian-acute-care-hospitals-2014-2018.html.
30. Public Health Agency of Canada. (2021) Hand Hygiene Practices in Healthcare Settings. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/nosocomial-occupational-infections/hand-hygiene-practices-healthcare-settings.html.
31. Public Health Agency of Canada. (2022). Healthcare-associated infections and antimicrobial resistance in acute care hospitals in Canada, 2016–2020. Canada Communicable Disease Report 48(7). Available from: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2022-48/issue-7-8-july-august-2022/healthcare-associated-infections-antimicrobial-resistance-canadian-acute-care-hospitals-2016-2020.html.
32. Reddy, S., Valerrama, A. & Kuhar, D. (2019). Improving the Use of Personal Protective Equipment: Applying Lessons Learned. Clinical Infectious Diseases 69(3): S165-S170. DOI: https://doi.org/10.1093/cid/ciz619.
33. Shadadi, H., Sheyback, M., Balouchi, A. & Shoorvazi, M. (2018). The barriers of clinical education in nursing: A systematic review. Biomedical Research 29(19):3616-3623. DOI: 10.4066/biomedicalresearch.29-18-1064.
34. Smith, L.E., Serfioti, D., Weston, D., Greenberg, N. & Rubin, G.J. (2021). Adherence to protective measures among healthcare workers in the UK: a cross-sectional study. Emergency Medicine Journal 39(2):100-105. DOI: 10.1136/emermed-2021-211454.
35. Tawfiq, J. & Auwaerter, P. (2019). Healthcare associated infections: the hallmark of Middle East respiratory syndrome coronavirus with review of the literature.
Journal of Hospital Infection 101(1):20-29. DOI: 10.1016/j.jhin.2018.05.021.
36. Van Gulik, N., Bouchoucha, S., Apivanich, S., Lucas, J. & Hutchinson, A. (2021). Factors influencing self-reported adherence to standard precautions among Thai nursing students: A cross sectional study. Nurse Education in Practice 57:103232. DOI: 10.1016/j.nepr.2021.103232.
37. Williams, V.R. et al. (2019). Improving healthcare worker adherence to the use of transmission-based precautions through application of human factors design: a prospective multi-centre study. Journal of Hospital Infection 103(1): 101-105. DOI: https://doi.org/10.1016/j.jhin.2019.03.014.
38. World Health Organisation. (2022). Global Report on Infection Prevention and Control. Available from: https://www.who.int/publications/i/item/9789240051164.


