Jennifer Happe, MSc1*, Nalini Agnihotri, PhD, CIC1,3, Jean Clark, RN, CIC4,5, Davenna Conrod, RN, BN4,6, Kevin Duran, RN, MD, CIC1,7,
Betty Ann Elford, RN, BN4,8, Shawna Ferenc, RN, BN4,9, Yvette Gable, RN, BN2,4, Kasey Gambeta, RN, MN, CIC4,10, Debora Giese, BSc, MScPH, CIC1,11,
Robin Johnson, MLT, BMLS, CIC4,7, Megan Lee, RN, BN4,12, Tammy MacDonald, RN, BScN, MBA, CIC1,13, Bois Marufov, MSc, MD, CIC1,
Katherine Paphitis, BSc, BASc, MSc, CPHI(C), CIC1,10, Dana Scott, RN, BN, BSc4,6, Ashley Shackleford, BHSc, CIC4,14, Betty Soanes, RN, GNC(C), CIC2,4
1 Infection Prevention and Control Canada (IPAC Canada) Surveillance and Applied Epidemiology Interest Group, IPAC Canada
2 Alberta Health Services, AB, Canada
3 Halton Healthcare, ON, Canada
4 IPAC Canada Long-Term Care Interest Group, Canada
5 Revera Inc., ON, Canada
6 Winnipeg Regional Health Authority, MB, Canada
7 Saskatchewan Health Authority, SK, Canada
8 Western Health, NL, Canada
9 Interlake-Eastern Regional Health Authority, MB, Canada
10 Public Health Ontario, ON, Canada
11 Northern Health, BC, Canada
12 Yukon Government Health and Social Services, YT, Canada
13 Nova Scotia Health, NS, Canada
14 Covenant Health, AB, Canada
*Corresponding author:
Jennifer Happe
Infection Prevention and Control Canada (IPAC Canada)
Surveillance and Applied Epidemiology Interest Group, IPAC Canada
Email: saeig@ipac-canada.org
ABSTRACT
Infection surveillance case definitions for the elderly in long-term care settings were published by Infection Prevention and Control Canada in 2017.
An expert consensus panel updated these definitions based on review of the current scientific literature.
KEYWORDS
surveillance; definitions; long-term care home
INTRODUCTION
Infectious disease surveillance in long-term care homes (LTCH) is essential to understand the burden of disease, detect outbreaks, and to inform infection prevention and control (IPAC) measures, including the implementation and monitoring of interventions aimed at reducing disease transmission. Infection presentation in the elderly may be atypical and surveillance case definitions developed for acute care settings may not be suitable (Stone et al., 2012). Members of the Infection Prevention and Control Canada (IPAC Canada) Surveillance and Applied Epidemiology Interest Group and Long-Term Care Interest Group formed a workgroup to review and update the 2017 IPAC Canada surveillance case definitions for infections that commonly occur in the elderly residing in LTCH, including respiratory tract infections, urinary tract infections, skin and soft tissue infections, and gastrointestinal infections (Happe et al., 2017). The goal is to maintain definitions that reflect current scientific literature.
Infection definitions herein are intended for surveillance purposes, and should not be used to guide clinical treatment. As infection presentation in the elderly may be atypical, failure to meet these surveillance definitions may not necessarily exclude the presence of a clinical infection. When applying the definitions, rule out non-infectious causes of signs and symptoms first and ensure that signs and symptoms are new or acutely worse than a resident’s baseline. It is recommended to closely monitor residents demonstrating early signs and symptoms of infection to detect cases promptly and make informed decisions about IPAC measures.
LTCHs often have limited resources available for surveillance. Therefore, it is recommended that surveillance programs focus on infections with the most potential for prevention, transmissibility, incidence, morbidity, and/or mortality. Attribution of an infection to an LTCH for surveillance purposes should occur if there is no evidence the infection was incubating on admission to the facility and if infection onset occurs more than or equal to three days after admission to the facility (CNISP, 2020; NHSN, 2023). Surveillance definitions should be applied in the context of a surveillance protocol which supports a standardized approach to collecting, analyzing, and reporting data used to inform IPAC policy and practices. Applying standardized case definitions ensures consistent and accurate surveillance data and allows comparison of data over time within a LTCH and between LTCHs at the local, provincial, territorial, and federal levels. Surveillance definitions should be reviewed periodically for accuracy and specificity. Surveillance reports should indicate when definitions are modified as this may influence the interpretation of surveillance data and the ability to compare data within an LTCH and externally. In 2020, IPAC Canada published an open access LTC Surveillance Toolkit which supports the entire surveillance process, including how to assess whether a LTCH is ready to conduct surveillance, how to implement a surveillance system, staff training tools, standardized data collection tools, and a Microsoft Excel™ database to store and analyze data (IPAC Canada, 2020).
The database autogenerates tables and figures for reports.
Finally, it is recommended to apply the Canadian Nosocomial Infection Surveillance Program (CNISP) surveillance definitions for infections in adults not included in this definition set, e.g., blood stream infections, Clostridioides difficile infections and COVID-19.
METHODS
The Centers for Disease Prevention and Control Healthcare Infection Control Practices Advisory Committee guideline development methodology was used to revise the definitions (Umscheid et al., 2010). This included a structured review of evidence found in peer-reviewed primary research reports, systematic reviews, and meta-analyses between 2016 and 2022. Literature was evaluated with the Public Health Agency of Canada Critical Appraisal Toolkit (Moralejo et al., 2017). Changes to case definitions were determined by consensus between workgroup members and reviewed by content experts, including infectious disease physicians, epidemiologists, infection control professionals and public health officials.
DEFINITIONS
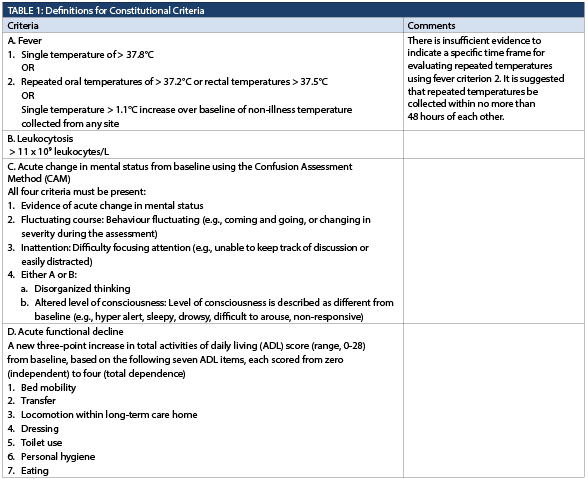
Constitutional criteria
No changes were made to the constitutional criteria in Table 1 as recent literature supports the existing definitions (El Chakhtoura et al., 2017; Jump et al., 2018; Mlinac et al., 2016; Rowe et al., 2022; Rudolph et al., 2020). However, the confusion assessment method (CAM) criteria, previously presented in a standalone table, have been enfolded into Table 1. CAM conducted by trained personnel remains the preferred method of confusion assessment due to its sensitivity, specificity, and objectivity (Bellelli et al., 2021; Jeong et al., 2020; Shenkin et al., 2019; Shi et al., 2013; Tieges et al., 2021a; Tieges et al., 2021b).
Respiratory tract infections
Respiratory tract infection definitions in Table 2 were scrutinized following the COVID-19 pandemic. The literature does not support a unique definition for identifying COVID-19 cases in the elderly, and it is recommended to use the general COVID-19 definition published by CNISP (Hunt et al., 2021; Khan et al., 2020; Millar et al., 2022; Zazzara et al., 2021). Common cold and influenza-like illness definitions were merged into a single, inclusive upper respiratory tract infection category (Andrew et al., 2020; Branche et al., 2016; Casalegno et al., 2017; Kodama et al., 2017; Talbot, 2017). No data were found to support changes to the pneumonia and lower respiratory tract definitions (Aronen et al., 2019; Metlay and Waterer, 2020).
Urinary tract infections
Urinary tract infection definitions are provided in Table 3.
A blood culture isolate positive for the same species of organism identified in a urine specimen, without an alternate site of infection, was previously considered a urinary tract infection (UTI). This criterion was removed after careful consideration since it is not possible to distinguish between asymptomatic bacteriuria and a UTI without considering the presence of signs and symptoms of a UTI (Moore et al., 2017; Haayman and Stobberingh, 2018; Ryan et al., 2018). Clarification was added on the timeframe within which all criteria used to identify a UTI must be met (NHSN, 2023).
Skin, soft tissue, and mucosal infections
Skin, soft tissue and mucosal infections definitions are provided in Table 4. Editorial changes to the comments were made for clarity. No data were found to support revisions of the definitions (Jump et al., 2018; Bennett et al., 2019; Engelman et al., 2020; Esposito et al., 2018; Lipsky et al., 2017; Osti et al., 2019; Poulakou et al., 2019; Thompson et al., 2017; Welch et al., 2021; Yogo et al., 2016).
Gastrointestinal tract infections
The gastrointestinal tract infection definition set in Table 5 was modified to include a single definition of gastroenteritis, which is inclusive of norovirus, instead of a separate definition for norovirus (Kirk et al., 2010; Sidoti et al., 2015; White et al., 2019. Additionally, Clostridium difficile was updated to Clostridioides difficile to reflect a recent reclassification of the bacterium (Diseases, 2019). It is recommended to closely monitor residents demonstrating early signs and symptoms of infection who may not meet surveillance definitions to detect individual cases and potential outbreaks promptly.